Purity: ≥98%
| ln Vitro |
p-Cresol inhibited MPAG formation in a potent and competitive manner (Ki=5.2 µM in pooled human liver microsomes) and the interaction was primarily mediated by UGT1A9. This interaction was estimated to increase plasma MPA exposure in patients by approximately 1.8-fold, which may result in MPA toxicity. The mechanism of inhibition for AcMPAG formation was noncompetitive (Ki=127.5 µM) and less likely to be clinically significant. p-Cresol was the most potent inhibitor of MPA-glucuronidation compared with other commonly studied uremic toxins (eg, indole-3-acetic acid, indoxyl sulfate, hippuric acid, kynurenic acid, and 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid) and its metabolites (ie, p-cresol sulfate and p-cresol glucuronide).[1]
|
|---|---|
| ln Vivo |
After oral administration of tyrosine feed to PBC (primary biliary cholangitis) mice, PCS (p-Cresol sulfate) increased, liver inflammatory factors were decreased, and anti-inflammatory factors were increased. Furthermore, Kupffer cells in the liver polarized form M1 transitioned to M2. PCS can damage normal bile duct epithelial cells and suppress the immune response of Kupffer cells. But PCS protects bile duct epithelial cells damaged by LPS through Kupffer cells.[2]
|
| Enzyme Assay |
Mycophenolic acid (MPA) is commonly prescribed for preventing graft rejection after kidney transplantation. The primary metabolic pathways of MPA are hepatic glucuronidation through UDP-glucuronosyltransferase (UGT) enzymes in the formation of MPA-glucuronide (MPAG, major pathway) and MPA-acyl glucuronide (AcMPAG). p-Cresol, a potent uremic toxin known to accumulate in patients with renal dysfunction, can potentially interact with MPA via the inhibition of glucuronidation. We hypothesized that the interaction between MPA and p-cresol is clinically relevant and that the estimated exposure changes in the clinic are of toxicological significance. Using in vitro approaches (ie, human liver microsomes and recombinant enzymes), the potency and mechanisms of inhibition by p-cresol towards MPA glucuronidation were characterized. Inter-individual variabilities, effects of clinical co-variates, in vitro-in vivo prediction of likely changes in MPA exposure, and comparison to other toxins were determined for clinical relevance. p-Cresol inhibited MPAG formation in a potent and competitive manner (Ki=5.2 µM in pooled human liver microsomes) and the interaction was primarily mediated by UGT1A9. This interaction was estimated to increase plasma MPA exposure in patients by approximately 1.8-fold, which may result in MPA toxicity. The mechanism of inhibition for AcMPAG formation was noncompetitive (Ki=127.5 µM) and less likely to be clinically significant. p-Cresol was the most potent inhibitor of MPA-glucuronidation compared with other commonly studied uremic toxins (eg, indole-3-acetic acid, indoxyl sulfate, hippuric acid, kynurenic acid, and 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid) and its metabolites (ie, p-cresol sulfate and p-cresol glucuronide). Our findings indicate that the interaction between p-cresol and MPA is of toxicological significance and warrants clinical investigation.[1]
|
| Cell Assay |
Gas chromatography-mass spectrometry (GC-MS) was used to detect differences in tyrosine, phenylalanine, tryptophan, PCS, and p-Cresyl glucuronide (PCG) between the serum of PBC patients and healthy controls. In vivo experiments, mice were divided into the normal control, PBC group, and PBC tyrosine group. GC-MS was used to detect PCS and PCG. Serum and liver inflammatory factors were compared between groups along with the polarization of liver Kupffer cells. Additionally, PCS was cultured with normal bile duct epithelial cells and Kupffer cells, respectively. PCS-stimulated Kupffer cells were co-cultured with lipopolysaccharide-injured bile duct epithelial cells to detect changes in inflammatory factors.[2]
|
| Animal Protocol |
Levels of tyrosine and phenylalanine were increased, but PCS level was reduced in PBC patients, with PCG showing a lower concentration distribution in both groups. PCS in PBC mice was also lower than those in normal control mice. After oral administration of tyrosine feed to PBC mice, PCS increased, liver inflammatory factors were decreased, and anti-inflammatory factors were increased. Furthermore, Kupffer cells in the liver polarized form M1 transitioned to M2. PCS can damage normal bile duct epithelial cells and suppress the immune response of Kupffer cells. But PCS protects bile duct epithelial cells damaged by LPS through Kupffer cells.[2]
|
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion
Humans normally excrete approximately 50 mg of p-cresol in the urine daily. p-Cresol is produced endogenously from tyrosine by anaerobic bacteria in the gastrointestinal tract. The normal human excretes 16 to 39 mg p-cresol/day. Cresols are slightly more corrosive /to the skin or eyes/ than phenol, but systemic effects may be a little milder because of slower absorption. Healthy humans excrete an average of about 50 mg (range 16-74 mg) of p-cresol in the urine daily. Endogenous p-cresol is produced from tyrosine, an amino acid present in most proteins, by anaerobic bacteria in the intestine. Free p-cresol formed in this way is absorbed from the intestine and eliminated in the urine as conjugates. For more Absorption, Distribution and Excretion (Complete) data for p-CRESOL (9 total), please visit the HSDB record page. Metabolism / Metabolites p-Cresol fed to rabbits is excreted in the urine as the glucuronide (60%) and sulfate (15%) conjugates, some 10% is oxidized to p-hydroxybenzoic acid and a trace is hydroxylated to 3,4-dihydroxytoluene. p-Cresol yields p-cresyl-beta-d-glucuronide, p-cresyl sulfate, p-hydroxybenzyl alcohol, 4-methylcatechol, and p-methylanisole in rabbits. p-Cresol yields p-cresyl sulfate in man. p-Cresol yields p-cresyl sulfate and p-methylanisole in rats. For more Metabolism/Metabolites (Complete) data for p-CRESOL (18 total), please visit the HSDB record page. 4-Methylphenol has known human metabolites that include 4-Methyl-2,5-cyclohexadien-1-one, (2S,3S,4S,5R)-3,4,5-Trihydroxy-6-(4-methylphenoxy)oxane-2-carboxylic acid, 4-methyl-hydroquinone, and 4-Hydroxybenzyl alcohol. 4-Methylphenol is a known human metabolite of toluene. Cresols can be absorbed following inhalation, oral, and dermal exposure. Once in the body they can distribute rapidly into many organs and tissues. Cresols undergo oxidative metabolism in the liver and are rapidly eliminated, mostly in the urine, as sulfate or glucuronide conjugates. The activation of cresols by oxidation involves tyrosinase and thyroid peroxidase, forming a reactive quinone methide. Experiments with recombinant P-450s demonstrated cresol metabolism was mediated by several P-450s including CYP2D6, 2C19, 1A2, 1A1, and 2E1. (L528, A197, L529, A198) |
| Toxicity/Toxicokinetics |
Toxicity Summary
IDENTIFICATION AND USE: p-Cresol is a crystalline solid below 95 °F. It has been used in explosive, petroleum, photographic, paint and agricultural industries, for making synthetic resins; in disinfectants and fumigants; as industrial solvent. p-Cresol is used in the formulation of antioxidants. p-Cresol has many applications in the fragrance and dye industries. Synthetic food flavors also contain p-cresol. It is used as local antiseptic, parasiticide, disinfectant in veterinary. HUMAN EXPOSURE AND TOXICITY: p-Cresol, an end product of aromatic amino acids, is produced from food proteins by intestinal bacteria, and is detectable in blood, urine and feces. p-Cresol may contribute to atherosclerosis and thrombosis in patients with uremia. Higher serum levels of p-cresol in chronic kidney disease populations have been associated with increased cardiovascular mortality. p-Cresol reduced the spontaneous contraction rates of cardiomyocytes, and caused irregular cardiomyocyte beating. In acute p-cresol-poisoning and long-term exposure to cresol as in severe uremic patients, p-cresol may potentially inhibit blood clot formation and lead to hemorrhagic disorders via inhibition of platelet aggregation. p-Cresol may play a role in the immune defect of uremic patients. Studies on the induction of unscheduled DNA synthesis showed p-cresol to be positive in human lung fibroblast cells in the presence of hepatic homogenates. ANIMAL STUDIES: p-Cresol can cause severe local irritation and corrosion following dermal and ocular exposure. Glaucoma has been induced experimentally in rabbits & monkeys by injection of 0.5-1.0% p-cresol emulsion in physiologic saline into the anterior chamber. Application of 0.5% p-cresol to the skin for 6 weeks resulted in permanent depigmentation of the skin and hair in black and agouti mice. All three cresols isomers are more toxic to mice than to rats when administered by gavage. o-Cresol is the most toxic, followed by p-cresol and then m-cresol. The effects are similar to, but less severe than, those following phenol exposure. Phenol, o- and p-cresol have about equal toxicity in cats while m-cresol is slightly less toxic. 180-280 mg/kg of p-cresol given iv to rabbits in a single dose, resulted in convulsions, coma, and death. In a 28-day study, rats and mice of both sexes were given p-cresol at concentrations of 300 to 30,000 ppm in the diet. All rats survived until study termination; some mice died at the 10,000 and 30,000 ppm dietary levels. Increased liver weights and kidney weights were noted in both species at doses as low as 3000 ppm. Bone marrow hyperplasia, and atrophy of the uterus, ovary, and mammary gland were seen in the 10,000- and 30,000-ppm dietary groups. In a 90-day study, rats were gavaged with 50, 175, or 600 mg p-Cresol/kg bw. The treatment with the highest dose caused combined mortality and significant reduction in bw and food consumption; CNS effects included lethargy, ataxia, coma, dyspnea, tremor, and convulsions within 15-30 min after dosing. A detailed oral neurotoxicity study of intermediate duration was performed on rats using all three cresol isomers. A host of clinical observations indicative of neurotoxicity (including hypoactivity, rapid labored respiration, excessive salivation, and tremors) was reported at doses of 50 mg/kg/day or higher for all three isomers. Convulsions were reported at 450 mg/kg/day or higher. Fetotoxicity was observed at parenterally-toxic doses in two-generation reproduction studies in rats. In a study conducted on cultured rat embryos in vitro, p-cresol caused dose-related effects on growth and structural abnormalities. p-Cresol caused an increased estrus cycle length in rats at 7500 and 30,000 mg/kg; there were no effects on the estrus cycle in mice. Female mice were dosed with a single application of dimethylbenzanthracene followed 1 wk later by 25uL of a 20% solution of p-cresol in benzene twice weekly for 12 wk. p-Cresol produced 7/20 tumors (papillomas) on surviving mice. p-Cresol given in the feed produced an increased incidence of mild and moderate hyperplasia of the forestomach of hamsters exposed for 20 weeks. P-Cresol was not genotoxic in vivo and in vitro. ECOTOXICITY STUDIES: A waterborne concn of 0.028 mM p-cresol resulted in statistically significant increases in serum sorbitol dehydrogenase activities shown by rainbow trout after 96 hr of exposure. During a 48-hr pulsed exposure to 8 mg p-cresol/L, the mortality of walleyed pike was very high. Smallmouth bass showed visible stress; largemouth bass showed no visible stress but had stopped feeding. The effects of p-cresol were examined on benthic macroinvertebrate flora and fauna in an EPA outdoor experimental stream facility located at Monticello, Minnesota. The primary effect of p-cresol was on the photosynthetic and respiration processes of aquatic plants. p-Cresol is a cholinesterase or acetylcholinesterase (AChE) inhibitor. A cholinesterase inhibitor (or 'anticholinesterase') suppresses the action of acetylcholinesterase. Because of its essential function, chemicals that interfere with the action of acetylcholinesterase are potent neurotoxins, causing excessive salivation and eye-watering in low doses, followed by muscle spasms and ultimately death. Nerve gases and many substances used in insecticides have been shown to act by binding a serine in the active site of acetylcholine esterase, inhibiting the enzyme completely. Acetylcholine esterase breaks down the neurotransmitter acetylcholine, which is released at nerve and muscle junctions, in order to allow the muscle or organ to relax. The result of acetylcholine esterase inhibition is that acetylcholine builds up and continues to act so that any nerve impulses are continually transmitted and muscle contractions do not stop. Among the most common acetylcholinesterase inhibitors are phosphorus-based compounds, which are designed to bind to the active site of the enzyme. The structural requirements are a phosphorus atom bearing two lipophilic groups, a leaving group (such as a halide or thiocyanate), and a terminal oxygen. Toxicity Data LC50 (rat) > 710 mg/m3/1hr LD50: 207 mg/kg (Oral, Rat) (T13) LD50: 301 mg/kg (Dermal, Rabbit) (T13) LD50: 25 mg/kg (Intraperitoneal, Mouse) (T13) Interactions /LABORATORY ANIMALS: Chronic Exposure or Carcinogenicity/ Mice were given a single dermal application of 9,10-dimethyl-1,2-benzanthracene (DMBA), a cancer initiator, followed by application of 20% solutions of o-, p-, or m-cresol in benzene twice a week for 12 weeks. This level of cresols exposure proved to be acutely toxic, producing relatively high nontumor-related mortality. Consequently, all tumor results were based on number of survivors (14-20 per group). Promotion with cresols led to increases in the average number of skin papillomas per mouse and the percentage of exposed mice with at least one papilloma. o-Cresol was the most potent isomer, and p-cresol the least. Carcinomas were not observed following cresols exposure, although the observed papillomas have the potential to develop into carcinomas. A problem with the study was use of benzene, a known carcinogen, as the solvent for the cresols. However, benzene controls in the cresols experiment did not develop papillomas, and neither did benzene controls in four parallel series of experiments (a few papillomas were observed in a fifth benzene control group). Therefore, the results of this study showing that all three cresol isomers are capable of promoting skin tumors initiated by DMBA appear to be valid. P-cresol is a well-known uremic toxin and environmental toxicant that may affect platelet functions. In this study, p-cresol (1-5 uM) inhibited the arachidonic acid (AA)-induced platelet aggregation, with 47% and 82% of inhibition at concentrations of 2 and 5 uM, respectively. Under similar experimental condition, p-cresol showed little effect on the U46619-induced platelet aggregation. p-cresol (<500 uM) revealed no discernable cytotoxicity to platelets as analyzed by quantification of lactate dehydrogenase release. Antiplatelet effect of p-cresol was related to inhibition of thromboxane A(2) (TXA(2)) and prostaglandin D(2) (PGD(2)) formation. P-cresol (2-100 uM) partly inhibited the AA-induced reactive oxygen species (ROS) production as well as the extracellular signal-regulated kinase (ERK1/2) and p38 phosphorylation in platelets. P-cresol further inhibited the AA-induced aggregation of rabbit platelet-rich plasma (PRP) with an IC50 of 2 uM and aggregation of human PRP (IC50 = 13.6 uM). Intravenous administration of p-cresol (250-1000 nmole) into mice effectively suppressed the ex vivo platelet aggregation, whereas showed little effect on the value of RBC, hemoglobin (HGB), hematocrit, MCV, MCH, MCHC, platelets and lymphocyte counts. These results indicate that in acute p-cresol-poisoning and long-term exposure to cresol as in severe uremic patients, p-cresol may potentially inhibit blood clot formation and lead to hemorrhagic disorders via inhibition of platelet aggregation, ROS production, ERK/p38 activation and TXA(2) production. ... DNA adduct formation in myeloperoxidase containing HL-60 cells treated with the toluene metabolite p-cresol /was examined/. Treatment of HL-60 cells with the combination of p-cresol and H2O2 produced four DNA adducts 1: (75.0%), 2: (9.1%), 3: (7.0%) and 4: (8.8%) and adduct levels ranging from 0.3 to 33.6 x 10-7. The levels of DNA adducts formed by p-cresol were dependent on concentrations of p-cresol, H2O2 and treatment time. In vitro incubation of p-cresol with myeloperoxidase and H2O2 produced three DNA adducts 1: (40.5%), 2: (28.4%) and 3: (29.7%) with a relative adduct level of 0.7x10-7. The quinone methide derivative of p-cresol (PCQM) was prepared by Ag(I)O oxidation. Reaction of calf thymus DNA with PCQM produced four adducts 1: (18.5%), 2: (36.4%), 3: (29.0%) and 5: (16.0%) with a relative adduct level 1.6x10-7. Rechromatography analyses indicates that DNA adducts 1-3 formed in HL-60 cells treated with p-cresol and after myeloperoxidase activation of p-cresol were similar to those formed by reaction of DNA with PCQM. This observation suggests that p-cresol is activated to a quinone methide intermediate in each of these activation systems. Taken together, these results suggest PCQM is the reactive intermediate leading to the formation of DNA adducts in HL-60 cells treated with p-cresol. Furthermore, the DNA adducts formed by PCQM may provide a biomarker to assess occupational exposure to toluene. Non-Human Toxicity Values LD50 Rat dermal 750 mg/kg LD50 Rat oral 207 mg/kg LD50 Rat oral 1.8 g/kg LD50 Mouse intraveneously 1460 mg/kg For more Non-Human Toxicity Values (Complete) data for p-CRESOL (12 total), please visit the HSDB record page. |
| References |
[1]. Toxicol Sci. 2020 Feb 1;173(2):267-279.
[2]. Cells. 2022 Nov 26;11(23):3782. |
| Additional Infomation |
P-cresol is a colorless solid with a tar like odor. Sinks and mixes slowly with water. (USCG, 1999)
P-cresol is a cresol that consists of toluene substituted by a hydroxy group at position 4. It is a metabolite of aromatic amino acid metabolism produced by intestinal microflora in humans and animals. It has a role as a uremic toxin, a human metabolite and an Escherichia coli metabolite. p-Cresol is a metabolite found in or produced by Escherichia coli (strain K12, MG1655). P-Cresol has been reported in Artemisia macrocephala, Viburnum cylindricum, and other organisms with data available. p-Cresol (4-methylphenol), a 108.1 Da volatile low-molecular-weight compound, is a phenol. It is a partially lipophilic moiety which strongly binds to plasma protein (close to 100%) under normal conditions. p-Cresol is metabolized through conjugation, mainly sulphation and glucuronization, but removal of the unconjugated p-cresol is, at least in part, via the urine. Therefore it is not surprising that this compound, together with several other phenoles, is retained when the kidneys fail. P-Cresol is an end-product of protein breakdown, and an increase of the nutritional protein load in healthy individuals results in enhanced generation and urinary excretion. The serum p-cresol concentration in uremic patients can be decreased by changing to a low-protein diet. p-Cresol is one of the metabolites of the amino acid tyrosine, and to a certain extent also of phenylalanine, which are converted to 4-hydroxyphenylacetic acid by intestinal bacteria, before being decarboxylated to p-cresol (putrefaction). The main contributing bacteria are aerobes (mainly enterobacteria), but to a certain extent also anaerobes play a role (mainly Clostridium perfringens). In uremia, modifications in the intestinal flora result in the specific overgrowth of bacteria that are specific p-cresol producers. The administration of antibiotics reduces urinary excretion of p-cresol, as a result of the liquidation of the producing bacteria. Environmental factors might also contribute. The liver cytochrome P450 metabolizes toluene to benzyl alcohol, but also to o-cresol and p-cresol. Toluene is not only used industrially, but it is also the most widely abusively inhaled solvent. Furthermore, p-cresol is a metabolite of menthofuran, one of the metabolites of R-(+)-pulegone, which is found in extracts from the plants Mentha pulegium and Hedeoma pulegioides, commonly known as pennyroyal oil and pennyroyal tea. These extracts are popular as unconventional herbal therapeutic agents and are applied as abortiva, diaphoretics, emmenagogues, and psychedelic drugs. Pennyroyal oil is extensively used for its pleasant mint-like smell in the flavoring industry. The toxicity of pennyroyal oil and menthofuran is well known. Another compound used in traditional medicine, especially in Japan, which is a precursor of p-cresol is wood tar creosote. p-Cresol has been reported to affect several biochemical, biological and physiological functions: (i) it diminishes the oxygen uptake of rat cerebral cortex slices; (ii) it increases the free active drug concentration of warfarin and diazepam; (iii) it has been related to growth retardation in the weanling pig; (iv) it alters cell membrane permeability, at least in bacteria; (v) it induces LDH leakage from rat liver slices; (vi) it induces susceptibility to auditive epileptic crises; and (vii) it blocks cell K+ channels. (A7723). p-Cresol is a uremic toxin that is at least partially removed by peritoneal dialysis in haemodialysis patients, and has been involved in the progression of renal failure. (MID: 11169029). At concentrations encountered during uremia, p-cresol inhibits phagocyte function and decreases leukocyte adhesion to cytokine-stimulated endothelial cells. (A3274). See also: Cresol (annotation moved to). Therapeutic Uses MEDICATION (VET): Local antiseptic, parasiticide, disinfectant; has been used as an intestinal antiseptic Disinfectant |
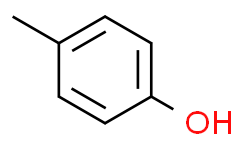
| Molecular Formula |
C7H8O
|
|---|---|
| Molecular Weight |
108.14
|
| Exact Mass |
108.057
|
| Elemental Analysis |
C, 77.75; H, 7.46; O, 14.79
|
| CAS # |
106-44-5
|
| Related CAS # |
27289-34-5;1121-70-6 (hydrochloride salt);72269-62-6 (aluminum salt)
|
| PubChem CID |
2879
|
| Appearance |
Crystalline solid [Note: A liquid above 95 degees F]
|
| Density |
1.0±0.1 g/cm3
|
| Boiling Point |
202.0±0.0 °C at 760 mmHg
|
| Melting Point |
32-34 °C(lit.)
|
| Flash Point |
81.0±8.2 °C
|
| Vapour Pressure |
0.2±0.4 mmHg at 25°C
|
| Index of Refraction |
1.546
|
| LogP |
1.94
|
| Hydrogen Bond Donor Count |
1
|
| Hydrogen Bond Acceptor Count |
1
|
| Rotatable Bond Count |
0
|
| Heavy Atom Count |
8
|
| Complexity |
62.8
|
| Defined Atom Stereocenter Count |
0
|
| SMILES |
CC1=CC=C(C=C1)O
|
| InChi Key |
IWDCLRJOBJJRNH-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C7H8O/c1-6-2-4-7(8)5-3-6/h2-5,8H,1H3
|
| Chemical Name |
4-methylphenol
|
| Synonyms |
NSC-3696; NSC 3696; p-Cresol
|
| HS Tariff Code |
2934.99.9001
|
| Storage |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| Solubility (In Vitro) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples.
Injection Formulations
Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline)(e.g. IP/IV/IM/SC) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). View More
Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] Oral Formulations
Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). View More
Oral Formulation 3: Dissolved in PEG400 (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 9.2473 mL | 46.2364 mL | 92.4727 mL | |
| 5 mM | 1.8495 mL | 9.2473 mL | 18.4945 mL | |
| 10 mM | 0.9247 mL | 4.6236 mL | 9.2473 mL |
*Note: Please select an appropriate solvent for the preparation of stock solution based on your experiment needs. For most products, DMSO can be used for preparing stock solutions (e.g. 5 mM, 10 mM, or 20 mM concentration); some products with high aqueous solubility may be dissolved in water directly. Solubility information is available at the above Solubility Data section. Once the stock solution is prepared, aliquot it to routine usage volumes and store at -20°C or -80°C. Avoid repeated freeze and thaw cycles.
Calculation results
Working concentration: mg/mL;
Method for preparing DMSO stock solution: mg drug pre-dissolved in μL DMSO (stock solution concentration mg/mL). Please contact us first if the concentration exceeds the DMSO solubility of the batch of drug.
Method for preparing in vivo formulation::Take μL DMSO stock solution, next add μL PEG300, mix and clarify, next addμL Tween 80, mix and clarify, next add μL ddH2O,mix and clarify.
(1) Please be sure that the solution is clear before the addition of next solvent. Dissolution methods like vortex, ultrasound or warming and heat may be used to aid dissolving.
(2) Be sure to add the solvent(s) in order.