
| Size | Price | Stock | Qty |
|---|---|---|---|
| 500mg |
|
||
| 1g |
|
||
| 5g |
|
||
| 10g |
|
||
| 25g |
|
||
| Other Sizes |
|
Purity: ≥98%
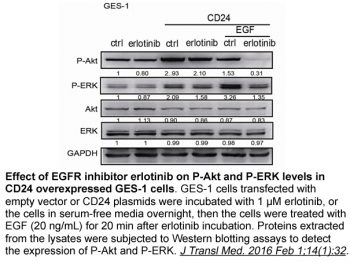
Erlotinib (formerly OSI744, trade name: Tarceva) is a quinazoline-based EGFR (epidermal growth factor receptor) inhibitor with potential antineoplastic activity. In cell-free experiments, it inhibits EGFR with an IC50 of 2 nM, and compared to human c-Src or v-Abl, it is >1000 times more sensitive to EGFR. Pancreatic cancer, non-small cell lung cancer (NSCLC), and various other cancers can be treated with erlotinib, a medication that has FDA approval. It inhibits EGFR phosphorylation and prevents the signal transduction pathways and carcinogenic consequences linked to EGFR activation by competing with adenosine triphosphate and reversibly binding to the intracellular catalytic domain of EGFR tyrosine kinase.
| Targets |
EGFR (IC50 = 2 nM)
|
|---|---|
| ln Vitro |
Erlotinib (CP-358774) is also a potent inhibitor, with an IC50 of 1 nM, of the EGFR's recombinant intracellular (kinase) domain. Erlotinib severely inhibits the proliferation of DiFi cells, with an IC50 of 100 nM for an 8-day proliferation assay[1]. When B-DIM and Erlotinib (2 μM) are combined, BxPC-3 cell colony formation is significantly inhibited as opposed to when either agent is used alone. Only in BxPC-3 cells does the combination of B-DIM and Erlotinib (2 μM) significantly induce apoptosis when compared to the apoptotic effect of either agent alone[2].
The epidermal growth factor receptor (EGFR) is overexpressed in a significant percentage of carcinomas and contributes to the malignant phenotype. CP-358,774 is a directly acting inhibitor of human EGFR tyrosine kinase with an IC50 of 2 nM and reduces EGFR autophosphorylation in intact tumor cells with an IC50 of 20 nM. This inhibition is selective for EGFR tyrosine kinase relative to other tyrosine kinases we have examined, both in assays of isolated kinases and whole cells. At doses of 100 mg/kg, CP-358,774 completely prevents EGF-induced autophosphorylation of EGFR in human HN5 tumors growing as xenografts in athymic mice and of the hepatic EGFR of the treated mice. CP-358,774 inhibits the proliferation of DiFi human colon tumor cells at submicromolar concentrations in cell culture and blocks cell cycle progression at the G1 phase. This inhibitor produces a marked accumulation of retinoblastoma protein in its underphosphorylated form and accumulation of p27KIP1 in DiFi cells, which may contribute to the cell cycle block. Inhibition of the EGFR also triggers apoptosis in these cells as determined by formation of DNA fragments and other criteria. These results indicate that CP-358,774 has potential for the treatment of tumors that are dependent on the EGFR pathway for proliferation or survival. [1] Effects of B-DIM and Erlotinib on the Viability of Pancreatic Cancer Cells [2] It is important to note that, during our pilot studies, as indicated in Materials and Methods, different concentrations of B-DIM and erlotinib were used and are presented in Table 1. Moreover, after analyzing the basal level of expression of EGFR, NF-κB, and COX-2, we chose two cell lines having constitutively activated levels of NF-κB, EGFR, and COX-2 expression (BxPC-3) compared with lower level of NF-κB, EGFR, and COX-2 expression (MIAPaCa). Our results prompted us to select the subsequent concentration of B-DIM and erlotinib as presented below. Cell viability of BxPC-3 and MIAPaCa pancreatic cancer cells treated with B-DIM (20 µmol/L), erlotinib (2 µmol/L), and the combination was determined by the MTT assay, and the data are presented in Fig. 1A and B. Significant inhibition of cell viability was seen in BxPC-3 cells treated with either agent, and this was further enhanced by the combination treatment (P = 0.0001). In addition, we have also tested the effects of treatment on cell viability by clonogenic assay as shown below. Similar treatments of MIAPaCa cells resulted in a significant inhibition of viable cells with B-DIM alone but not when exposed to similar concentrations of B-DIM and erlotinib for the same time, and the effect was not enhanced by the combination treatment (P = 0.0890). The insensitivity of MIAPaCa cells to erlotinib is consistent with a recently published report Inhibition of Cell Growth/Survival by Clonogenic Assay [2] To determine the effect of B-DIM and Erlotinib on cell growth, cells were treated with each of the single agents or their combination and assessed for cell viability by clonogenic assay. The combination of B-DIM and erlotinib resulted in a significant inhibition of colony formation in BxPC-3 cells when compared with either agent alone (Fig. 2A and B). Similar treatment of MIAPaCa cells (Fig. 2C) showed inhibition of colony formation with B-DIM alone and also the combination, but the effect was not enhanced with the combination treatment as was seen in BxPC-3 cells (Fig. 2A and B). These results were similar to those obtained from the soft-agar assay. Overall, the results from clonogenic assay was consistent with the MTT data as shown in Fig. 1A and B, suggesting that B-DIM had a differential effect between BxPC-3 and MIAPaCa pancreatic cancer cells. The mechanisms of such differences were further investigated, and the results are presented in the following sections, but first we have determined the effects of B-DIM, erlotinib, and the combination on apoptotic cell death. Induction of Apoptosis by Erlotinib, B-DIM, and the Combination [2] The underlying mechanism on the inhibition of cell viability was further studied by determining the apoptotic effects of different treatments using the Cell Death Detection ELISA. The combination of B-DIM and erlotinib resulted in a significant induction of apoptosis only in BxPC-3 cells when compared with the apoptotic effect of either agent alone (Fig. 1C). Similar treatment of MIAPaCa cells showed no induction of apoptosis with the combination (Fig. 1D). These results are consistent with cell viability assay by MTT. Subsequently, we sought to find further evidence of apoptosis as presented below. B-DIM Enhances Apoptosis Signaling by Erlotinib [2] PARP cleavage was determined in BxPC-3 and MIAPaCa cells that were treated with B-DIM (20 µmol/L), erlotinib (2 µmol/L), and the combination (Fig. 3). We found significant amount of PARP (116 kDa) protein cleavage product (85 kDa fragment) after 72-h treatment only in BxPC-3 cells (Fig. 3). In contrast, MIAPaCa cells treated similarly showed only a small cleavage of PARP with B-DIM alone and also in combination but not with erlotinib alone. The induction of apoptosis could be partly due to inactivation of important survival genes; hence, we investigated whether B-DIM, erlotinib, and their combination could affect key survival proteins. Effect of B-DIM on Molecules Related to Apoptosis [2] BxPC-3 and MIAPaCa cells were used to evaluate the effects of B-DIM and/or Erlotinib on the expression of survivin, Bcl-2, Bcl-xL, and c-IAP1/2. Expression of Bcl-2, Bcl-xL, survivin, and c-IAP1/2 proteins was significantly reduced in cells treated with the combination when compared with either agent alone (Fig. 3). There was no influence on antiapoptotic proteins in MIAPaCa cells treated with either agent alone or the combination. These results suggest that B-DIM, erlotinib, and the combination down-regulate key survival proteins and in turn induced apoptotic cell death in BxPC-3 cells but not in MIAPaCa cells. To further determine the molecular mechanism by which B-DIM sensitized BxPC-3 cells to erlotinib-induced inhibition of cell viability and induction of apoptosis, we investigated the role of EGFR and its downstream signaling pathways. Effect of B-DIM on the Expression of EGFR Protein [2] The expression of EGFR was determined by immunoblotting. No baseline expression of EGFR was found in the MIAPaCa cells. EGFR-expressing BxPC-3 cells showed a significant reduction in the expression of EGFR and phosphorylated EGFR levels when exposed to erlotinib plus B-DIM compared with either agent alone (Fig. 3). It is known that the activation of EGFR could in turn regulate an important transcription factor, NF-κB, which is a known regulator of several survival genes such as survivin, c-IAP1/2, Bcl-2, and Bcl-xL. Because we found a greater degree of down-regulation of survivin, c-IAP1/2, Bcl-2, and Bcl-xL in BxPC-3 cells treated with B-DIM and erlotinib compared with either agent alone, and because these genes are transcriptionally regulated by NF-κB, we investigated the effect of each treatment on the DNA-binding activity of NF-κB. B-DIM Inhibits NF-κBDNA-Binding Activity [2] The activation of NF-κB, a nuclear transcriptional factor, was assessed in B-DIM-treated and Erlotinib-treated cells. There was a significant inhibition of NF-κB activation in BxPC-3 cells exposed to both erlotinib and B-DIM compared with erlotinib alone (Fig. 4A). No such inhibition was shown in the MIAPaCa cells (Fig. 4B). These results suggest that the combination of B-DIM and erlotinib causes greater inhibition of cell growth, induction of apoptosis, inhibition of survival factors, inhibition of EGFR, and inactivation of NF-κB. Because NF-κB plays important roles in the regulation of prosurvival and antiapoptotic processes, we tested whether overexpression of NF-κB by p65 cDNA transfection could abrogate B-DIM-induced and erlotinib-induced apoptotic processes. Moreover, it is known that NF-κB transcriptionally regulates COX-2, which produces PGE2 and in turn induces cell viability. Thus, we tested whether celecoxib, erlotinib, or B-DIM alone could influence the activity of B-DIM and erlotinib in p65 cDNA transfected cells. Erlotinib, B-DIM, and Celecoxib Abrogated Activation of NF-κBActivity Stimulated by p65 cDNA Transfection [2] Cytoplasmic and nuclear proteins from BxPC-3 and MIAPaCa cells transfected with p65 cDNA and then treated with erlotinib (2 µmol/L), B-DIM (20 µmol/L), or celecoxib (5 µmol/L) or left untreated for 48 h were subjected to analysis for NF-κB activity as measured by Western blot analysis and EMSA. The results showed that erlotinib, B-DIM, and celecoxib inhibited the p65 protein and NF-κB DNA-binding activity more in BxPC-3 cells compared with untreated cells (Fig. 5A and B) and very little effect was seen in MIAPaCa cells. Importantly, NF-κB p65 cDNA transfection enhanced the NF-κB p65 protein and DNA-binding activity only in BxPC-3 cells to a significant level as shown in Fig. 5A and B. On the other hand, no such changes were observed in the MIAPaCa cells. Because the activation of NF-κB induces COX-2 expression leading to the production of PGE2 that is released into the culture medium, we measured the levels of PGE2 in untransfected and transfected cells treated with erlotinib, B-DIM, and the COX-2 inhibitor celecoxib. Inhibition of PGE2 Synthesis in p65 cDNA-Transfected Cells [2] We measured the levels of PGE2 in the conditioned medium collected from both BxPC-3 and MIAPaCa cells as an indicator of COX-2 activity. We found a high level of PGE2 secretion by BxPC-3 cells, whereas MIAPaCa cells showed very low levels of PGE2, which is consistent with its low constitutive expression of COX-2. BxPC-3 and MIAPaCa cells were transfected with p65 cDNA followed by treatment with Erlotinib (10 nmol/L), B-DIM (1 µmol/L), or celecoxib (1 nmol/L) to analyze the levels of PGE2 released into the culture medium (Fig. 5C). No change in PGE2 level was noted when cells were treated with erlotinib alone (P = 0.084). However, a significant reduction in PGE2 level was observed in BxPC-3 cells treated with B-DIM (P = 0.006) and celecoxib (P = 0.005). There was a substantial increase in the PGE2 level in p65 cDNA-transfected BxPC-3 cells compared with untransfected cells (P = 0.009), suggesting that NF-κB could induce COX-2 expression. However, there was no change in PGE2 level in MIAPaCa cells with any of the agents. Collectively, these results suggest that the production of PGE2 is mediated through the NF-κB and COX-2 pathway and that celecoxib could down-regulate both NF-κB and COX-2. These results were subsequently correlated with the degree of apoptosis (Fig. 5D) as presented below. Apoptosis through the Inactivation of NF-κB in p65 cDNA-Transfected Cells [1] p65 cDNA was transfected into BxPC-3 and MIAPaCa cells and then treated with Erlotinib (2 µmol/L), B-DIM (20 µmol/L), or celecoxib (5 µmol/L) for 48 h (Fig. 5D). The degree of apoptosis in p65 cDNA-transfected BxPC-3 cells treated with erlotinib (P = 0.034) was much less compared with untransfected cells treated with erlotinib (P = 0.007). Similar results were observed with both B-DIM and celecoxib treatment in BxPC-3 cells. However, in MIAPaCa cells, no such degree of apoptosis was observed. These results suggest that activation of NF-κB by p65 cDNA transfection could abrogate the apoptosis inducing effect of erlotinib, B-DIM, and celecoxib. |
| ln Vivo |
In comparison to the untreated control, the combination of B-DIM and Erlotinib (50 mg/kg, i.p.) treatment significantly (P <0.01) reduces tumor weight under experimental conditions[2]. In comparison to the CP+vehicle (V) rats, erlotinib (20 mg/kg, p.o.) significantly attenuates the body weight (BW) loss induced by Cisplatin (CP) (P<0.05). Treatment with erlotinib considerably enhances renal function in CP-N (normal control group, NC) rats. Compared to the CP+V rats, the CP+Erlotinib (E) rats exhibit a significant increase in urine volume (UV) (P<0.05) and Cr clearance (Ccr) (P<0.05), as well as a significant decrease in serum creatinine (s-Cr) (P<0.05), blood urea nitrogen (BUN) (P<0.05), and urinary N-acetyl-β-D-glucosaminidase (NAG) index (P<0.05).
B-DIM Augments In vivo Therapeutic Effect of Erlotinib on Primary Tumor [2] Potential therapeutic utility of B-DIM and erlotinib combination in SCID mice bearing orthotopically implanted BxPC-3 pancreatic tumor cells was investigated. A dose of 3.5 mg/d B-DIM per mouse was selected for p.o. administration, whereas erlotinib dose (50 mg/kg body weight i.p.) was based on previously published reports as shown in Fig. 6A. A total of 28 mice were divided into four groups. To ascertain the efficacy of a single-agent treatment compared with combinations, we determined the mean pancreas weight in all treated groups. Under our experimental conditions, administration of B-DIM by gavage treatment and erlotinib alone caused 20% and 35% reduction in tumor weight, respectively, compared with control tumors (Fig. 6C). However, under the experimental conditions, the combination of B-DIM and erlotinib treatment showed significant decrease (P < 0.01) in tumor weight compared with untreated control, B-DIM alone, or erlotinib alone treatment group. These results showed, for the first time, the efficacy of combination of B-DIM and erlotinib in the inhibition of pancreatic tumor growth in an orthotopic model. B-DIM Inhibits NF-κBDNA-Binding Activity In vivo [2] The activation of NF-κB was assessed in B-DIM-treated and Erlotinib-treated tumor tissues. The results show that NF-κB was down-regulated by B-DIM and erlotinib (Fig. 6B). Fig. 6B (bottom) represents results from all seven mice. These in vivo results were similar to our in vitro findings, suggesting that the inactivation of NF-κB is, at least, one of the molecular mechanisms by which B-DIM potentiates erlotinib-induced antitumor activity in our experimental animal model. The effects of blocking the epidermal growth factor receptor (EGFR) in acute kidney injury (AKI) are controversial. Here we investigated the renoprotective effect of Erlotinib, a selective tyrosine kinase inhibitor that can block EGFR activity, on cisplatin (CP)-induced AKI. Groups of animals were given either Erlotinib or vehicle from one day before up to Day 3 following induction of CP-nephrotoxicity (CP-N). In addition, we analyzed the effects of erlotinib on signaling pathways involved in CP-N by using human renal proximal tubular cells (HK-2). Compared to controls, rats treated with erlotinib exhibited significant improvement of renal function and attenuation of tubulointerstitial injury, and reduced the number of apoptotic and proliferating cells. Erlotinib-treated rats had a significant reduction of renal cortical mRNA for profibrogenic genes. The Bax/Bcl-2 mRNA and protein ratios were significantly reduced by erlotinib treatment. In vitro, we observed that erlotinib significantly reduced the phosphorylation of MEK1 and Akt, processes that were induced by CP in HK-2. Taken together, these data indicate that erlotinib has renoprotective properties that are likely mediated through decreases in the apoptosis and proliferation of tubular cells, effects that reflect inhibition of downstream signaling pathways of EGFR. These results suggest that erlotinib may be useful for preventing AKI in patients receiving CP chemotherapy[3]. |
| Enzyme Assay |
The kinase reaction takes place in 50 μL of 50 mM HEPES (pH 7.3), which also contains 15 ng of affinity-purified EGFR from A431 cell membranes, 1.6 μg/mL EGF, 0.1 mM Na3VO4, 125 mM NaCl, and 20 μM ATP. To achieve a final DMSO concentration of 2.5%, the compound is added to DMSO. The addition of ATP starts the phosphorylation process, which lasts for 8 mm at room temperature while being constantly shaken. The reaction mixture is aspirated to stop the kinase reaction, and wash buffer is used four times over. Phosphorylated PGT is quantified after 25 microseconds of incubation with 50 microliters of HRP-conjugated PY54 antiphosphotyrosine antibody per well, diluted to 0.2 micrograms/mL in blocking buffer (PBS containing 3% BSA and 0.05% Tween 20). After aspirating out the antibody, the plate is cleaned four times using wash buffer. TMB Microwell Peroxidase Substrate, 50 μL per well, is added to develop the colonmetric signal.0.09 M sulfuric acid, 50 μL per well, is added to stop the signal. The absorbance at 450 nm is used to estimate phosphotyrosine. The signal for controls is proportional to the incubation time for 10 mm and usually ranges from 0.6 to 1.2 absorbance units[1]. In wells devoid of AlP, EGFR, or POT, there is essentially no background signal.
|
| Cell Assay |
In order to assess the survival of cells treated with B-DIM, Erlotinib, or both, 3,000–5,000 BxPC-3 and MIAPaCa cells are plated per well in a 96-well plate and incubated at 37°C for the entire night. Initially, B-DIM (10-50 µM) and Erlotinib (1-5 µM) are tested at a range of concentrations. The concentrations of B-DIM (20 µM) and Erlotinib (2 µM) are selected for each assay based on the preliminary findings. The standard MTT assay is used to measure the effects of B-DIM (20 µM), Erlotinib (2 µM), and the combination on BxPC-3 and MIAPaCa cells. The assay is performed three times after 72 hours. The Tecan microplate fluorometer measures the color intensity at 595 nm. Cells treated with DMSO are given a value of 100% and are regarded as the untreated control. We have performed clonogenic assay in addition to the aforementioned assay to evaluate the effects of treatment[2].
Cell Viability Assay [2] To test the viability of cells treated with B-DIM, Erlotinib, or the combination, BxPC-3 and MIAPaCa cells were plated (3,000–5,000 per well) in a 96-well plate and incubated overnight at 37°C. We initially tested a range of concentrations for both B-DIM (10–50 µmol/L) and erlotinib (1–5 µmol/L). Based on the initial results, the concentration of B-DIM (20 µmol/L) and erlotinib (2 µmol/L) were chosen for all assays. The effects of B-DIM (20 µmol/L), erlotinib (2 µmol/L), and the combination on BxPC-3 and MIAPaCa cells were determined by the standard 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay after 72 h and was repeated three times. The color intensity was measured by a Tecan microplate fluorometer at 595 nm. DMSO-treated cells were considered to be the untreated control and assigned a value of 100%. In addition to the above assay, we have also done clonogenic assay for assessing the effects of treatment as shown below. Clonogenic Assay [2] To test the survival of cells treated with B-DIM, Erlotinib, or the combination, BxPC-3 and MIAPaCa cells were plated (50,000–100,000 per well) in a six-well plate and incubated overnight at 37°C. After 72-h exposure to 20 µmol/L B-DIM, 2 µmol/L erlotinib, and the combination, the cells were trypsinized, and the viable cells were counted (trypan blue exclusion) and plated in 100 mm Petri dishes in a range of 100 to 1,000 cells to determine the plating efficiency as well as assess the effects of treatment on clonogenic survival. The cells were then incubated for ~10 to 12 days at 37°C in a 5% CO2/5% O2/90% N2 incubator. The colonies were stained with 2% crystal violet and counted. The surviving fraction was normalized to untreated control cells with respect to clonogenic efficiency, which was 83% for both BxPC-3 and MIAPaCa cells. In addition to this assay, cells were also treated similarly and plated in soft-agar (soft-agar colony assay) and incubated at 37°C. The colonies in the soft agar were also counted in all untreated and treated wells after 12 days. Quantification of Apoptosis by ELISA [2] The Cell Death Detection ELISA kit (Roche Applied Science) was used to detect apoptosis in untreated and treated BxPC-3 and MIAPaCa cells. Cells seeded in six-well plates were treated with B-DIM (20 µmol/L), Erlotinib (2 µmol/L), or the combination. The cells were trypsinized and ~10,000 cells were used as described earlier. Tecan microplate fluorometer was used to measure color intensity at 405 nm. The experiment was repeated three times. Protein Extraction and Western Blot Analysis [2] BxPC-3 and MIAPaCa cells treated with B-DIM (20 µmol/L), Erlotinib (2 µmol/L), or the combination for 72 h were used to evaluate the effects of treatment on survivin, Bcl-2, Bcl-xL, EGFR, EGFR-pTyr1173, c-IAP1/2, Src, poly(ADP-ribose) polymerase (PARP), and β-actin expression. The experiment was carried out for a minimum of three times. Cells were harvested as described previously. The samples were loaded on 7% to 12% SDSPAGE for separation and electrophoretically transferred to a nitrocellulose membrane. Each membrane was incubated with monoclonal antibody against survivin, Bcl-2, Bcl-xL, Src, c-IAP1/2, EGFR, EGFR-pTyr1173, PARP, and β-actin. Blots were incubated with secondary antibodies conjugated with peroxidase. The signal intensity was then measured using chemiluminescent detection system. Electrophoretic Mobility Shift Assay for NF-κB Activation [2] To evaluate the effect of B-DIM and Erlotinib on BxPC-3 and MIAPaCa cells, the cells were either untreated or treated with B-DIM (20 µmol/L), erlotinib (2 µmol/L), or the combination with a minimum repeat of experiment at least three times for 72 h. The cells or the minced tumor tissue were homogenized using a Dounce homogenizer in 400 µL ice-cold lysis buffer as described earlier. |
| Animal Protocol |
Mice: The treatment groups consist of seven randomly assigned female ICR-SCID mice, aged 6-7 weeks: (a) control (no treatment); (b) B-DIM (50 mg/kg body weight) administered intragastrically once daily; (c) Erlotinib (50 mg/kg body weight) administered daily intraperitoneally for 15 days; and (d) B-DIM and Erlotinib administered according to the schedule for individual treatments. After receiving their last dose of medication, all mice are killed on day three, and their body weight is recorded. A portion of the tissue is immediately frozen in liquid nitrogen and kept cold (−70°C) for later use, while the remaining portion is fixed in formalin and prepared for paraffin block processing. The presence of a tumor or tumors in each pancreas is verified by staining a fixed tissue section with H&E.
Rats: Male Sprague-Dawley (SD) rats six weeks of age, weighing 180–210 g, are utilized. On day 0, SD rats (n=28) receive an intraperitoneal injection of 7 mg/kg of freshly prepared ciprofloxacin (CP) at a concentration of 1 mg/mL. For the purpose of examining Erlotinib's effects, 28 CP-N rats are split into two groups. Animals in two groups (n = 14) are given daily oral gavages of either Erlotinib (20 mg/kg) (CP+E, n = 14) or vehicle (CP+V, n = 14) from day -1 (24 hours before the CP injection) to day 3. Groups treated with vehicles are given the same amount of saline. At six weeks of age, a normal control group (NC, n = 5) consists of five male SD rats. From the first to the third day, the NC rats receive an equivalent volume of saline orally via gavage. Day 4 (96 hours post-CP injection): rats are anesthetized, and following a cardiac puncture, they are sacrificed by exsanguination. The kidneys and blood are simultaneously extracted. Renal tissue is sectioned and fixed in 2% paraformaldehyde/phosphate-buffered saline (PBS) for later use, or it can be snap-frozen in liquid nitrogen. In order to reduce suffering as much as possible, diethyl ether gas anesthesia is used during all surgical procedures. Mice were randomized into the following treatment groups (n = 7): (a) untreated control; (b) only B-DIM (50 mg/kg body weight), intragastric once every day; (c) Erlotinib (50 mg/kg body weight), everyday i.p. for 15 days; and (d) B-DIM and Erlotinib, following schedule as for individual treatments. All mice were killed on day 3 following last dose of treatment, and their body weight was determined. One part of the tissue was rapidly frozen in liquid nitrogen and stored at −70°C for future use and the other part was fixed in formalin and processed for paraffin block. H&E staining of fixed tissue section was used to confirm the presence of tumor(s) in each pancreas. [2] Cisplatin (CP) was freshly prepared in saline at a concentration of 1 mg ml−1 and then injected intraperitoneally in SD rats (n = 28) at a dose of 7 mg/kg on day 0. The dose of CP was selected based on a previous stud. To investigate the effect of Erlotinib, 28 CP-N rats were divided into two groups. Separate groups (n = 14) each of animals were administered with either Erlotinib (20 mg/kg, Cugai Pharmaceutical/F. Hoffmann-La Roche, Basel, Switzerland) (CP+E, n = 14) or vehicle (CP+V, n = 14) daily by oral gavage from day -1 (24 hours prior to the CP injection) to day 3. Vehicle-treated groups received an equivalent volume of saline. Five male SD rats at the age of 6 weeks were used as a normal control group (NC, n = 5). The NC rats were given an equivalent volume of saline daily by oral gavage from day -1 to day 3. At day 4 (96 hours after CP injection), each rat was anesthetized and sacrificed by exsanguination after the cardiac puncture; blood was collected by cardiac puncture and kidneys were collected (Figure 1). Renal tissue was divided; separate portions were snap-frozen in liquid nitrogen or fixed in 2% paraformaldehyde/phosphate-buffered saline (PBS) for later use. All surgery was performed under diethyl ether gas anesthesia, and all efforts were made to minimize suffering. |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion
Erlotinib is about 60% absorbed after oral administration and its bioavailability is substantially increased by food to almost 100%. Peak plasma levels occur 4 hours after dosing. The solubility of erlotinib is pH dependent. Solubility decreases pH increases. Smoking also decrease the exposure of erlotinib. Following a 100 mg oral dose, 91% of the dose was recovered in which 83% was in feces (1% of the dose as unchanged parent compound) and 8% in urine (0.3% of the dose as unchanged parent compound). Apparent volume of distribution = 232 L Smokers have a 24% higher rate of erlotinib clearance. Erlotinib is about 60% absorbed after oral administration and its bioavailability is substantially increased by food to almost 100%. Peak plasma levels occur 4 hours after dosing. The solubility of erlotinib is pH dependent. Erlotinib solubility decreases as pH increases. Following absorption, erlotinib is approximately 93% protein bound to plasma albumin and alpha-1 acid glycoprotein. Erlotinib has an apparent volume of distribution of 232 liters. Time to reach steady state plasma concentration /is/ 7 - 8 days. No significant relationships of clearance to covariates of patient age, body weight or gender were observed. Smokers had a 24% higher rate of erlotinib clearance. Following a 100 mg oral dose, 91% of the dose was recovered: 83% in feces (1% of the dose as intact parent) and 8% in urine (0.3% of the dose as intact parent). For more Absorption, Distribution and Excretion (Complete) data for Erlotinib (10 total), please visit the HSDB record page. Metabolism / Metabolites Metabolism occurs in the liver. In vitro assays of cytochrome P450 metabolism showed that erlotinib is metabolized primarily by CYP3A4 and to a lesser extent by CYP1A2, and the extrahepatic isoform CYP1A1. Metabolism and excretion of erlotinib, an orally active inhibitor of epidermal growth factor receptor tyrosine kinase, were studied in healthy male volunteers after a single oral dose of (14)C-erlotinib hydrochloride (100-mg free base equivalent, approximately 91 microCi/subject)... In plasma, unchanged erlotinib represented the major circulating component, with the pharmacologically active metabolite M14 accounting for approximately 5% of the total circulating radioactivity. Three major biotransformation pathways of erlotinib are O-demethylation of the side chains followed by oxidation to a carboxylic acid, M11 (29.4% of dose); oxidation of the acetylene moiety to a carboxylic acid, M6 (21.0%); and hydroxylation of the aromatic ring to M16 (9.6%). In addition, O-demethylation of M6 to M2, O-demethylation of the side chains to M13 and M14, and conjugation of the oxidative metabolites with glucuronic acid (M3, M8, and M18) and sulfuric acid (M9) play a minor role in the metabolism of erlotinib. The identified metabolites accounted for >90% of the total radioactivity recovered in urine and feces. The metabolites observed in humans were similar to those found in the toxicity species, rats and dogs. Erlotinib has known human metabolites that include Erlotinib M14. Biological Half-Life Median half-life of 36.2 hours. A population pharmacokinetic analysis in 591 patients receiving the single-agent erlotinib hydrochloride 2nd/3rd line regimen showed a median half-life of 36.2 hours. |
| Toxicity/Toxicokinetics |
Hepatotoxicity
Elevations in serum aminotransferase levels are common during erlotinib therapy of pancreatic and lung cancers, and values above 5 times the upper limit of normal occur in at least 10% of patients. Similar rates of ALT elevations, however, can occur with comparable antineoplastic regimens. The abnormalities are usually asymptomatic and self-limited, but may require dose adjustment or discontinuation (Case 1). In addition, there have been rare reports of clinically apparent liver injury attributed to erlotinib therapy. The time to onset is typically within days or weeks of starting therapy, and the liver injury can be severe, there being at least a dozen fatal instances reported in the literature. The onset of injury can be abrupt and the pattern of serum enzyme elevations is usually hepatocellular (Case 2). Immunoallergic features (rash, fever and eosinophilia) are not common and autoantibody formation has not been reported. Routine monitoring of liver tests during therapy is recommended. The rate of clinically significant liver injury and hepatic failure is increased in patients with preexisting cirrhosis or hepatic impairment due to liver tumor burden. Likelihood score: B (likely but uncommon cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of erlotinib during breastfeeding. Because erlotinib is 93% bound to plasma proteins, the amount in milk is likely to be low. However, its half-life is about 36 hours and it might accumulate in the infant. It is also given in combination with gemcitabine for pancreatic cancer, which may increase the risk to the infant. The manufacturer recommends that breastfeeding be discontinued during erlotinib therapy and for 2 weeks after the final dose. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 93% protein bound to albumin and alpha-1 acid glycoprotein (AAG) Interactions Because cigarette smoking reduces systemic exposure to erlotinib, patients should be advised to stop smoking. If patients continue to smoke, an increase in erlotinib dosage may be considered; upon smoking cessation, dosage of erlotinib should be reduced immediately to the starting dose level. Drugs that increase the pH of the upper GI tract decrease the solubility of erlotinib and reduce its bioavailability.1 Concomitant administration of omeprazole, a proton pump inhibitor, decreased the area under the concentration-time curve for erlotinib by 46% and decreased the maximum concentration of erlotinib by 61%. Increasing the dose level of erlotinib is not likely to compensate for the loss of exposure, and separation of doses may not eliminate the interaction because proton pump inhibitors have an extended effect on the pH of the upper GI tract. If possible, the concomitant use of erlotinib and proton pump inhibitors should be avoided. The use of antacids may be considered as an alternative to histamine 2 receptor blockers or proton pump inhibitors in patients receiving erlotinib. However, the effect of antacids on the disposition of erlotinib has not been studied. If use of an antacid is necessary, the antacid dose and the erlotinib dose should be separated by several hours. Potential pharmacologic interaction (increased international normalized ratio [INR] and infrequent reports of bleeding, including GI and non-GI bleeding). Monitor prothrombin time (PT) or INR regularly in patients receiving erlotinib concomitantly with warfarin or other coumarin-derivative anticoagulants. For more Interactions (Complete) data for Erlotinib (7 total), please visit the HSDB record page. |
| References |
|
| Additional Infomation |
Therapeutic Uses
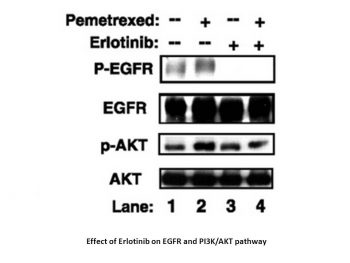
Erlotinib hydrochloride monotherapy is indicated for the maintenance treatment of patients with locally advanced or metastatic non-small cell lung cancer whose disease has not progressed after four cycles of platinum-based first-line chemotherapy. /Included in US product label/ Erlotinib hydrochloride monotherapy is indicated for the treatment of patients with locally advanced or metastatic non-small cell lung cancer after failure of at least one prior chemotherapy regimen. /Included in US product label/ Erlotinib hydrochloride in combination with gemcitabine is indicated for the first-line treatment of patients with locally advanced, unresectable or metastatic pancreatic cancer. /Included in US product label/ Drug Warnings The manufacturer states that there are no known contraindications to the use of erlotinib. Serious, sometimes fatal, interstitial lung disease-like events have occurred in patients receiving erlotinib. Interstitial lung disease-like events have been reported in approximately 0.7% of about 4900 patients receiving erlotinib in controlled and uncontrolled studies. In the principal efficacy study for non-small cell lung cancer, the reported incidence of interstitial lung disease-like events (0.8%) was similar among patients receiving erlotinib and those receiving placebo. In the principal efficacy study for pancreatic cancer, interstitial lung disease-like events occurred in 2.5% of patients receiving erlotinib and gemcitabine versus 0.4% of those receiving placebo and gemcitabine. Onset of manifestations occurred from 5 days to more than 9 months (median: 39 days) after initiating erlotinib therapy. Reported diagnoses in patients suspected of having interstitial lung disease-like events included pneumonitis, radiation pneumonitis, hypersensitivity pneumonitis, interstitial pneumonia, interstitial lung disease, obliterative bronchiolitis, pulmonary fibrosis, acute respiratory distress syndrome, and lung infiltration. Among patients receiving erlotinib for non-small cell lung cancer, most of these cases were associated with confounding or contributing factors, including concomitant or prior chemotherapy, prior radiotherapy, preexisting parenchymal lung disease, metastatic lung disease, or pulmonary infections. Interruption or discontinuance of erlotinib therapy may be required in patients experiencing pulmonary toxicity. Hepatorenal syndrome or acute renal failure, sometimes fatal, and renal insufficiency, with or without hypokalemia, have been reported in patients receiving erlotinib. Factors contributing to these adverse renal effects included baseline hepatic impairment; severe dehydration caused by diarrhea, vomiting, and/or anorexia; and concurrent chemotherapy. If dehydration occurs, erlotinib therapy should be interrupted and rehydration measures should be initiated. Periodic monitoring of renal function and serum electrolytes is recommended in patients at risk of dehydration. For more Drug Warnings (Complete) data for Erlotinib (27 total), please visit the HSDB record page. The epidermal growth factor receptor (EGFR) is overexpressed in a significant percentage of carcinomas and contributes to the malignant phenotype. CP-358,774 is a directly acting inhibitor of human EGFR tyrosine kinase with an IC50 of 2 nM and reduces EGFR autophosphorylation in intact tumor cells with an IC50 of 20 nM. This inhibition is selective for EGFR tyrosine kinase relative to other tyrosine kinases we have examined, both in assays of isolated kinases and whole cells. At doses of 100 mg/kg, CP-358,774 completely prevents EGF-induced autophosphorylation of EGFR in human HN5 tumors growing as xenografts in athymic mice and of the hepatic EGFR of the treated mice. CP-358,774 inhibits the proliferation of DiFi human colon tumor cells at submicromolar concentrations in cell culture and blocks cell cycle progression at the G1 phase. This inhibitor produces a marked accumulation of retinoblastoma protein in its underphosphorylated form and accumulation of p27KIP1 in DiFi cells, which may contribute to the cell cycle block. Inhibition of the EGFR also triggers apoptosis in these cells as determined by formation of DNA fragments and other criteria. These results indicate that CP-358,774 has potential for the treatment of tumors that are dependent on the EGFR pathway for proliferation or survival. [1] Blockade of epidermal growth factor receptor (EGFR) by EGFR tyrosine kinase inhibitors is insufficient for effective antitumor activity because of independently activated survival pathways. A multitargeted approach may therefore improve the outcome of anti-EGFR therapies. In the present study, we determined the effects of 3,3'-diindolylmethane (Bioresponse BR-DIM referred to as B-DIM), a formulated DIM with greater bioavailability on cell viability and apoptosis with erlotinib in vitro and in vivo using an orthotopic animal tumor model. BxPC-3 and MIAPaCa cells with varying levels of EGFR and nuclear factor-kappaB (NF-kappaB) DNA-binding activity were treated with B-DIM (20 micromol/L), erlotinib (2 micromol/L), and the combination. Cell survival and apoptosis was assessed by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide and histone-DNA ELISA. Electrophoretic mobility shift assay was used to evaluate NF-kappaB DNA-binding activity. We found significant reduction in cell viability by both 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide and clonogenic assays, induction of apoptosis, down-regulation of EGFR phosphorylation, NF-kappaB DNA-binding activity, and expression of antiapoptotic genes in BxPC-3 cells when treated with the combination of erlotinib and B-DIM compared with either agent alone. In contrast, no such effect was observed in MIAPaCa cells by similar treatment. Most importantly, these in vitro results were recapitulated in animal model showing that B-DIM in combination with erlotinib was much more effective as an antitumor agent compared with either agent alone. These results suggest that the utilization of B-DIM could be a useful strategy for achieving better treatment outcome in patients with activated status of EGFR and NF-kappaB in their tumors. [2] With respect to limitations of this study, we must consider several issues. First, food intake was not controlled among the three groups. Since the animals were not pair fed, it was hard to determine whether BW loss was depending on low intake or influence of CP induced AKI itself. Second, the present study did not address tubular dysfunction including salt and magnesium wasting, which is one of the most common physiological abnormalities associated with CP-N. Third, the therapeutic effect of erlotinib on recovery phase from CP-induced AKI was not investigated. Clinically, therapeutic effect on recovery phase as well as preventive effect on early phase is thought to be relevant to patients receiving CP chemotherapy. Lastly, the influence of erlotinib on antitumorigenic effects of CP was not proved. Further studies to evaluate whether the reduction of CP-elicited cell death by erlotinib was specific for the kidney by using different tumor cell lines like previous studies are needed. In conclusion, our in vivo and in vitro studies show that erlotinib has a renoprotective effect in CP-N, an effect that might be attributable to the attenuation of the apoptosis and proliferation of proximal tubular cells. Protection by erlotinib appears to be mediated through the inhibition of downstream signaling of EGFR, including MAPK and PI3K-Akt. These results suggest that erlotinib may be useful for preventing AKI in patients receiving CP chemotherapy.[3] |
| Molecular Formula |
C22H23N3O4
|
|---|---|
| Molecular Weight |
393.44
|
| Exact Mass |
393.168
|
| Elemental Analysis |
C, 67.16; H, 5.89; N, 10.68; O, 16.27
|
| CAS # |
183321-74-6
|
| Related CAS # |
Erlotinib Hydrochloride;183319-69-9;Erlotinib mesylate;248594-19-6;Erlotinib-d6;1034651-23-4;Erlotinib-13C6;1211107-68-4
|
| PubChem CID |
176870
|
| Appearance |
White to off-white crystalline powder
|
| Density |
1.2±0.1 g/cm3
|
| Boiling Point |
553.6±50.0 °C at 760 mmHg
|
| Melting Point |
223 - 228ºC
|
| Flash Point |
288.6±30.1 °C
|
| Vapour Pressure |
0.0±1.5 mmHg at 25°C
|
| Index of Refraction |
1.615
|
| LogP |
2.39
|
| Hydrogen Bond Donor Count |
1
|
| Hydrogen Bond Acceptor Count |
7
|
| Rotatable Bond Count |
11
|
| Heavy Atom Count |
29
|
| Complexity |
525
|
| Defined Atom Stereocenter Count |
0
|
| SMILES |
O(C([H])([H])C([H])([H])OC([H])([H])[H])C1C([H])=C2C(=NC([H])=NC2=C([H])C=1OC([H])([H])C([H])([H])OC([H])([H])[H])N([H])C1=C([H])C([H])=C([H])C(C#C[H])=C1[H]
|
| InChi Key |
AAKJLRGGTJKAMG-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C22H23N3O4/c1-4-16-6-5-7-17(12-16)25-22-18-13-20(28-10-8-26-2)21(29-11-9-27-3)14-19(18)23-15-24-22/h1,5-7,12-15H,8-11H2,2-3H3,(H,23,24,25)
|
| Chemical Name |
N-(3-ethynylphenyl)-6,7-bis(2-methoxyethoxy)quinazolin-4-amine
|
| Synonyms |
Erlotinib free base; NSC718781; NSC718781; CP358774; OSI-774; OSI 774; NSC 718781; CP-358,774; CP-358774; OSI774
|
| HS Tariff Code |
2934.99.9001
|
| Storage |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| Solubility (In Vitro) |
|
|||
|---|---|---|---|---|
| Solubility (In Vivo) |
Solubility in Formulation 1: 10 mg/mL (25.42 mM) in 50% PEG300 + 50% Saline (add these co-solvents sequentially from left to right, and one by one), suspension solution; with sonication.
Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: 10 mg/mL (25.42 mM) in 0.5% CMC-Na/saline water (add these co-solvents sequentially from left to right, and one by one), suspension solution; with ultrasonication. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5417 mL | 12.7084 mL | 25.4168 mL | |
| 5 mM | 0.5083 mL | 2.5417 mL | 5.0834 mL | |
| 10 mM | 0.2542 mL | 1.2708 mL | 2.5417 mL |
*Note: Please select an appropriate solvent for the preparation of stock solution based on your experiment needs. For most products, DMSO can be used for preparing stock solutions (e.g. 5 mM, 10 mM, or 20 mM concentration); some products with high aqueous solubility may be dissolved in water directly. Solubility information is available at the above Solubility Data section. Once the stock solution is prepared, aliquot it to routine usage volumes and store at -20°C or -80°C. Avoid repeated freeze and thaw cycles.
Calculation results
Working concentration: mg/mL;
Method for preparing DMSO stock solution: mg drug pre-dissolved in μL DMSO (stock solution concentration mg/mL). Please contact us first if the concentration exceeds the DMSO solubility of the batch of drug.
Method for preparing in vivo formulation::Take μL DMSO stock solution, next add μL PEG300, mix and clarify, next addμL Tween 80, mix and clarify, next add μL ddH2O,mix and clarify.
(1) Please be sure that the solution is clear before the addition of next solvent. Dissolution methods like vortex, ultrasound or warming and heat may be used to aid dissolving.
(2) Be sure to add the solvent(s) in order.
Erlotinib, Gemcitabine and Nab-Paclitaxel in Advanced Pancreatic Cancer
CTID: NCT01010945
Phase: Phase 1 Status: Completed
Date: 2024-11-21
|
 |
 |