
| Size | Price | Stock | Qty |
|---|---|---|---|
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|
Purity: ≥98%
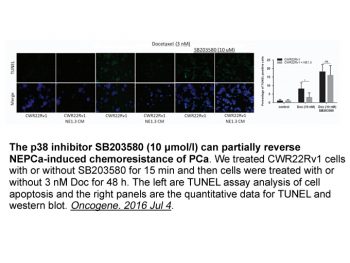
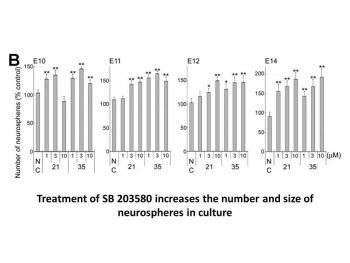
Adezmapimod (SB-203580; RWJ-64809; SB203580; RWJ 64809) is a novel and potent p38 mitogen-activated protein kinase inhibitor (p38MAPK inhibitor) that has the potential to treat Systemic lupus erythematosus (SLE). In THP-1 cells, it blocks PKB phosphorylation with an IC50 of 3-5 μM, inhibits p38MAPK with IC50s of 0.3-0.5 μM , and is 10-fold less potent than SAPK3(106T) and SAPK4(106T). By reducing proinflammatory cytokines and proteolytic factors in a mouse model, SB203580 inhibits the growth of endometriosis. With a Ki of 21 nM, SB203580 is a competitive ATPsite inhibitor of p38MAPK with selectivity likely influenced by nonconserved regions within or close to the ATP binding pocket.
| Targets |
p38 (IC50 = 50 nM); p38β2 (IC50 = 500 nM)
|
|---|---|
| ln Vitro |
SB203580 has an IC50 of 3-5 μm and inhibits the proliferation of murine CT6 T cells, BAF F7 B cells, or primary human T cells when IL-2 is present. Although the concentration needed is a little bit higher and the IC50 is above 10 μm, SB203580 also inhibits IL-2-induced p70S6 kinase activation. With an IC50 in the 3-10 μm range, SB203580 also inhibits the activity of PDK1 in a dose-dependent manner.[1] SB203580 has an IC50 of about 0.07 μm for blocking p38-MAPK stimulation of MAPKAPK2, whereas it has an IC50 of 3–10 μm for blocking total SAPK/JNK activity. Higher concentrations of SB203580 cause the ERK pathway to be activated, which then improves the transcriptional activity of NF-κB.[2] Human hepatocellular carcinoma (HCC) cells are induced to undergo autophagy by SB203580.[3]
SB203580 Inhibits IL-2-induced Rb Hyperphosphorylation [1] As we have shown previously, the IL-2-induced proliferation of primary human T cells, murine CT6 T cells, or BAF F7 B cells is prevented by the p38 MAP kinase inhibitor with an IC50 of 3–5 μm (Fig. 1). However, as our recent studies showed that IL-2-induced proliferation and the inhibitory effects of SB203580 on this event were independent of p38 MAP kinase or even p54 MAP kinase activity in both T cells and B cells, we endeavored to identify other possible targets involved in mediating the anti-proliferative effects. To do this, we investigated events associated with cell cycle progression. SB203580 had no effect on Myc expression, except for a small reduction at 30 μm only (Fig. 2 a). Furthermore, nuclear staining of SB203580-treated CT6 cells with propidium iodide showed no evidence of apoptosis after stimulation with IL-2 for 20 h (data not shown). The expression of hyperphosphorylated Rb and degradation of p27kip1 were also measured as markers of S-phase entry. The addition of IL-2 to resting CT6 cells caused the hyperphosphorylation of Rb as detected by Western blotting (Fig.2 b). The presence of SB203580 in the antiproliferative (0–30 μm) range resulted in a dose-dependent reduction in the hyperphosphorylated form (Fig. 2 b). There also appeared to be some reduction in the total levels of Rb protein. Similar inhibitory effects on Rb hyperphosphorylation and protein levels were obtained with wortmannin and LY294002, both inhibitors of PI 3-kinase. The decrease in Rb protein is likely to be due to the IL-1-converting enzyme (ICE)-mediated proteolysis of the hypophosphorylated form, which has been previously reported. These results would also agree with previous studies on the role of PI 3-kinase in IL-2-induced Rb hyperphosphorylation and protein by Brennanet al. and would support previous indications that PI 3-kinase is a proximal regulator of Rb. The effects of SB203580 on Rb hyperphosphorylation were confirmed in similar studies on activated primary human T cells (Fig. 2 d). We also investigated a second cell cycle-regulated protein, p27kip1. The addition of IL-2 to resting CT6 cells induces the degradation of p27kip1(Fig. 2 c). This degradation was unaffected by SB203580, which if anything, further reduced levels of the protein. Wortmannin and LY294002 similarly had no inhibitory effect on p27kip1 degradation. Again, these studies on p27kip1 degradation were repeated in activated primary human T cells, with no significant inhibition observed with SB203580 or wortmannin, although LY294002 had some inhibitory effect (Fig. 2 e). SB203580 Inhibits the Phosphorylation and Activation of PKB [1] The characteristic, S-phase hyperphosphorylation of Rb induced by IL-2 has been reported to be mediated by the PI 3-kinase pathway via the distal effector PKB. Furthermore, both the mitogenic and survival functions of the PI 3-kinase pathway have, in several reports, been attributed to PKB. We were therefore interested in investigating the possibility that SB203580 mediates its effects on Rb by inhibiting these kinases, especially as wortmannin and LY294002 displayed similar effects. The activation of PKB requires the PI 3-kinase-generated second messenger PIP3 as well as phosphorylation on Thr308 and Ser473 mediated by the PIP3-dependent kinases, PDK1 and PDK2, respectively. We investigated the effect of SB203580 on PKB activation by looking at IL-2-induced phosphorylation of residue Ser473 of PKB in whole cell lysates using a phospho-specific antibody. In both CT6 and activated human T cells, SB203580 inhibited the phosphorylation of Ser473 in a dose-dependent manner (Fig.3, a and b). Similar studies on the IL-2-responsive BA/F3 F7 B cells gave the same result (Fig. 3 c). The approximate IC50 for the effect of SB203580 on this parameter is ∼5 μm, similar to the concentration required for the inhibitory effects on proliferation (Fig. 1). As expected, wortmannin (Fig. 3) and LY294002 (not shown) also inhibited Ser473 phosphorylation, whereas rapamycin (not shown) had no effect. The phosphorylation of PKB on Thr308 was similarly investigated. As the antibody was not so effective, PKB was first immunoprecipitated, and phospho-Thr308 was detected by Western blotting. SB203580 inhibited Thr308 phosphorylation in CT6 cells with similar efficacy to the Ser473 phosphorylation (Fig.4). Wortmannin, as expected, also inhibited this Thr308 phosphorylation. To confirm that the effects of SB203580 on PKB phosphorylation correlated with kinase activity, assays were performed on immunoprecipitated PKB from IL-2-stimulated CT6 cells (Fig. 5). The drug inhibited PKB activation with an IC50 of 3–10 μm, in agreement with its effects on phosphorylation of the kinase and cell proliferation. SB203580 Inhibits the Activation of p70S6 Kinase but Not PI 3-Kinase [1] Although the above results showed that PKB activation is inhibited, it is still possible that PKB is one of several mitogenic effector molecules downstream of the actual SB203580 target. Therefore the effect of SB203580 on IL-2-induced activation of the PI 3-kinase/PKB pathway was examined. Exposure of CT6 cells to IL-2 leads to a reproducible 2-fold increase in anti-p85-precipitable PI 3-kinase activity. This was unaffected by preincubating the cells with SB203580. In contrast, wortmannin totally inhibited this activity (Fig.6). Furthermore, direct addition of SB203580 to PI 3-kinase assays did not have any effect (results not shown), indicating that PI 3-kinase is not the target of the drug. The effect of SB203580 on PI 3-kinase/PKB pathway was also examined indirectly. Several studies have shown that p70S6 kinase is a distal mediator of PI 3-kinase activity in several systems. As expected, wortmannin (Fig. 6 b) and LY294002 (not shown) inhibited the activation of p70S6 kinase by IL-2, as measured in immunokinase assays. We observed that SB203580 could also inhibit IL-2-induced p70S6 kinase activation, although the concentration required was slightly higher with an IC50 above 10 μm. These observations place the target of SB203580 downstream of PI 3-kinase but upstream of p70S6 kinase. Furthermore, it suggests that the SB203580 target is a common activator of both PKB and p70S6 kinase. The most likely candidate is PDK1, which has been reported to phosphorylate and activate p70S6 kinase. The higher IC50 for p70S6 kinase activation may reflect the fact that PDK1 contributes to only one of several phosphorylations required for p70S6 kinase activation. SB203580 Can Act as an Inhibitor of PDK1 [1] The data so far suggest that PDK1 and/or PDK2, the PKB kinases, are possible targets for SB203580. The Thr308 kinase, PDK1, is a constitutively active enzyme, but the phosphorylation of PKB on Thr308 is regulated by PIP3. The kinase for Ser473, a putative PDK2, is so named because it is also dependent on PIP3, but PDK2 has not been fully characterized, and as a result, no direct assays are available to examine its activity. Because we had evidence that PI 3-kinase activity and, therefore, PIP3 production are not inhibited (Fig.6 a), we examined whether SB203580 could act as a PDK1 inhibitor. To do this, recombinant kinase was used with recombinant PKB as the substrate. Activity of the enzyme was assessed by measuring the incorporation of [32P]phosphate into PKB (Fig.7 a). SB203580 was able to inhibit the activity of PDK1 in a dose-dependent manner with an IC50 in the 3–10 μm range, but CNI-1493, an inhibitor of p38MAP kinase activation, did not affect PDK1 activity. The recombinant PKB used in this assay, but not the PDK1, had endogenous autokinase activity (results not shown), so we tested the effect of the drug on this (Fig. 7 b). SB203580 was unable to inhibit PKB autokinase activity. The inhibition of PDK1 by SB203580 identifies it as the putative target in the PI 3-kinase pathway, in agreement with its reported role in p70S6 kinase activation and supported by our finding above (Fig. 6 b). p38 MAP Kinase Is Not Involved in PKB Phosphorylation [1] Although the above data demonstrate that SB203580 is an inhibitor of the PKB kinases (PDK1 and by inference PDK2), it was important to discriminate between the effects of SB203580 on PKB activation and the p38 MAP kinase pathway. SB203580 at 1 μM and kinase-deficient MKK3 and MKK6 do not affect NF-κB transactivation potential [2] To analyse a possible correlation between p38 MAPK and NF-κB activation, pIL6(-122)luc-transfected TF-1 cells were pretreated with the p38 kinase specific inhibitor SB203580 prior to OA stimulation (Cuenda et al., 1995). SB203580 was utilized at a concentration of 1 μM, which was previously shown to greatly inhibit p38 kinase activity in TF-1 cells (Birkenkamp et al., 1999). Results demonstrated that SB203580 did not affect the OA-induced NF-κB-driven promoter activity (5.1±1.1 fold for SB203580 plus OA versus 4.5±0.6 fold for OA, n=6) (Figure 4A). SB203580 at 5 or 10 μM enhances NF-κB-mediated promoter activity, but not GAL4p65-driven promoter activity [2] In many reports concerning various cell types, SB203580 is applied at concentrations of 5 and 10 μM, at which it demonstrates considerable inhibitive effects (Bergmann et al., 1998; Cuenda et al., 1997). To rule out that the lack of effect of SB203580 is due to inadequate concentrations, pIL6(-122)luc-transfected cells were pretreated with 5 and 10 μM SB203580, prior to OA stimulation. Surprisingly, exposure to SB203580 at these concentrations enhanced rather than inhibited NF-κB DNA binding (Figure 1) as well as NF-κB-mediated gene transcription (Figure 6A). SB203580 at 5 μM plus OA resulted in a 8.5±1.2 fold induction of NF-κB-regulated promoter activity versus a 4.5±0.6 fold induction after stimulation with OA only (P<0.05, n=6) (Figure 6A). Similarly, when pretreated with SB203580 at 10 μM prior to OA, promoter activity was enhanced 9.1±1.6 fold (P<0.05, n=6), while SB203580 at 10 μM alone had no effect (1.0±0.2 fold) (Figure 6A). SB203580 at 10 μM enhances phosphorylation of ERK1/2 and JNK [2] The above-described results would suggest that the p38 MAP kinase specific inhibitor SB203580 activates rather than inhibits signalling molecules when applied at concentrations of 5 and 10 μM. Activation of these signalling modules may then result in the activation of gene transcription regulated by NF-κB. Previously, we demonstrated the involvement of the ERK1/2 and JNK MAP kinase pathways in mediating NF-κB-regulated gene transcription in TF-1 cells and monocytes (Tuyt et al., 1999). We thus set out to investigate whether SB203580 is capable of activating the ERK and JNK pathways, when utilized at 10 μM. TF-1 cells were stimulated with OA for 90 min or pretreated with 1 or 10 μM of SB203580 for 30 min prior to OA stimulation. Total cell lysates were separated on SDS–PAGE gels and analysed for phosphorylated ERK1/2 and phosphorylated JNK1/2. Total ERK and JNK protein were visualized for equal loading. As depicted in Figure 7 stimulation with OA resulted in considerable phosphorylation of both the ERK (Figure 7A) and JNK (Figure 7B) proteins. Pretreatment with 1 μM SB203580 did not affect the level of either phospho-ERK or phospho-JNK. However, when TF-1 cells were pretreated with 10 μM SB203580 prior to OA, both phospho-ERK and phospho-JNK levels were strongly enhanced when compared with OA stimulation (Figure 7). Kinase-inactive Raf-1 suppresses SB203580-enhanced NF-κB activity [2] Since SB203580 at 10 μM considerably activated the ERK1/2 and JNK pathways, we set out to investigate whether these pathways are also involved in SB203580-enhanced NF-κB activity. For this purpose, TF-1 cells were transiently transfected with pIL6(-122)luc together with kinase-deficient mutants of molecules belonging to the ERK1/2 (pRSV-NΔRaf1) (Schaap et al., 1993), JNK (pcDNA3-MKK4(Ala), and pcDNA3-Flag-JNK) (Whitmarsh et al., 1997), and p38 (pRSV-MKK3(Ala) and pcDNA3-MKK6(K82A)) (Raingeaud et al., 1996) MAP kinase pathways. After transfection, cells were treated with medium, OA or SB203580 at 5 μM for 30 min prior to OA exposure. Possible involvement of MAP kinase pathways was identified when the induction of NF-κB activity due to SB203580 treatment was suppressed in the presence of a dominant negative construct when compared with the SB203580-mediated induction after introduction of the empty vector. The results demonstrated that only pRSV-NΔRaf1 was capable of suppressing the SB203580-enhanced NF-κB transcriptional activity (Figure 8A). NF-κB-mediated gene transcription after SB203580 plus OA treatment was suppressed down to 66±5% after the introduction of pRSV-NΔRaf1 when compared with cotransfection with pcDNA3, which was set at 100% (P<0.05, n=3). Induction of autophagy by SB203580 [3] The autophagy was first assessed by observing the change in the cell morphology. After incubation with SB203580 for 24 h, the morphological evaluation under visible light revealed a significant increase in the number of HepG2 cells with autophagosomes (Fig. 1a) which were recognized as characteristic double-membrane vacuolar structures containing various kinds of cytoplasmic contents. Similar results were also observed in other HCC cells and Chang cells (supplemental Fig. 1). The occurrence of authophage was confirmed by the detection of GFP-LC3 dots. Compared with the control cells, SB203580-treated cells displayed more GFP-LC3 dots (Fig. 1b, c). The percentage of GFP-LC3-positive cells with GFP-LC3 punctate dots was increased in a dose-dependent manner after SB203580 treatment (Fig. 1b, c). In addition to autophagosomes and GFP-LC3 dots, the increased expression of LC3-II protein is another marker for autophagy. The level of LC3-II was increased by SB203580 in a dose-dependent manner (Fig. 1c). In order to check whether the apoptosis also occurred in SB203580-treated HCC cells, HepG2 cells were stained with Hoechst 33342 to detect apoptosis. The result did not show any typical characteristic of apoptosis in cells treated with SB203580. Moreover, PARP was not cleavaged in HepG2 cells treated with SB203580 (Fig. 1e), confirming the absence of apoptosis. As a positive control, we used etoposide, a known apoptotic inducer, to treat HepG2 cells, and the cells showed DNA condensation and cleavaged PARP (Fig. 1d, e), both of which are the characteristics of apoptosis. SB203580-induced autophagy was independent of p38 MAPK [3] In order to test the role of p38 MAPK in the SB203580-induced autophagy, we used siRNA to block the expression of p38 MAPK in HCC cells. It showed that siRNA treatment did not change the SB203580-induced autophagy (Fig. 2), suggesting that SB203580-induced autophagy was independent of p38 MAPK. Similar results were obtained when p38 MAPK activity was inhibited by BIRB0796, a special p38 MAPK inhibitor (supplemental Fig. 4). The p38 MAPK-independent autophagy induced by SB203580 was further confirmed by the over-expression experiment, in which cells were transfected with pcDNA3.1-p38 MAPK to enhance the level of p38 MAPK. p38 MAPK over-expression also failed to affect SB203580-induced autophagy (Supplemental Fig. 5). AMPK inhibitor compound C prevented SB203580-induced autophagy [3] It is well known that AMPK activation is involved in autophagy induction. We thus investigated whether AMPK could influence autophagic process induced by SB203580. The result demonstrated that SB203580 treatment increased the levels of pAMPK, S78/80-ACCα, LC3-II (Fig. 3d) and autophagosome (Fig. 3a), indicating the occurrence of autophagy. However, pre-treated with compound C, a cell-permeable pyrrazolopyrimidine derivative that functions as a potent ATP-competitive inhibitor of AMPK, significantly decreased the number of cells with autophagosome (Fig. 3a), and suppressed the levels of LC3-II, pAMPK and S78/80-ACCα (Fig. 3d). Furthermore, SB203580-induced GFP-LC3-positive cells with GFP-LC3 punctate dots were also reduced by compound C (Fig. 3b, c). We also showed that the level of pDAPK was increased but the expression of phosphorylated p53 (pp53) was decreased in presence of compound C (Fig. 3d). DAPK siRNA prevented SB203580-induced autophagy [3] Since DAPK plays a critical role in autophagy and this protein was activated (dephosphorylated) in SB203580-induced autophagy, we investigated the functional role of DAPK in SB203580-induced autophagy using DAPK siRNA. Our data showed that the decrease of DAPK alleviated SB203580-induced autophagy, evident by the changes in the cell morphology (Fig. 4a), the decreased percentage of GFP-LC3-positive cells with GFP-LC3 punctate dots (Fig. 4b, c), and the reduction of autophagosome (Fig. 4a) and LC3-II (Fig. 4d). These results confirm that DAPK plays a positive role in SB203580-induced HCC cell autophagy. Our data also showed that DAPK siRNA decreased the level of S20-p53 but did not affect the expression of S15-p53. These findings indicate that DAPK may help to phosphate p53 at S20 but not at S15. DAPK siRNA affected neither AMPK nor LC3-II (Fig. 4d). It was also noted that DAPK siRNA could not 100% prevent SB203580-induced autophagy (Fig. 4b, c), suggesting that molecules other than DAPK are also significant in the SB203580-induced autophagy. PFT-α and p53 siRNA inhibited SB203580-induced autophagy [3] Although SB203580 did not up-regulate total p53 level in HCC cells, the levels of S15-p53 and S20-p53 were increased (Fig. 1f). We examined how the downregulation of p53 affected SB203580-induced autophagy by inhibiting p53 with chemical and siRNA methods. Our result showed that inhibition of p53 by p53 siRNA significantly blocked SB203580-induced autophagy in HepG2 cells (Fig. 5). However, it did not inhibit SB203580-mediated dephosphorylated DAPK and pAMPK (Fig. 5d). The similar results were obtained when PFT-α, a well-known chemical inhibitor for p53 [26], was used (Supplemental Fig. 6). These data suggest that p53 is involved in the autophagy induced by SB203580 and that AMPK and DAPK are likely to function upstream of p53 in SB203580-induced autophagy (Fig. 6). |
| ln Vivo |
SB203580 protects pig myocardium in an in vivo model from ischemic damage.[4] SB203580 is effective at both preventing and treating Systemic Lupus Erythematosus (SLE) in MRL/lpr mice.[5]
Proteinuria is prevented in SB203580 treated MRL/lpr mice. [5] ALT and AST are not influenced by SB203580 in MRL/lpr mice. [5] BUN but not Cr is decreased in SB203580 treated MRL/lpr mice. Renal but not splenic weight is reduced in SB203580 treated MRL/lpr mice. [5] Renal pathologic changes are attenuated in SB203580 treated MRL/lpr mice. [5] Hepatic pathologic changes are relieved in SB203580 treated MRL/lpr mice. [5] Splenic pathologic changes are relieved in SB203580 treated MRL/lpr mice. [5] Glomerular IgG, IgM, IgA and C3 depositions are reduced in SB203580 treated MRL/lpr mice. [5] The effect of SB203580 infusion on infarct size [4] The effects of local and systemic infusions of the p38-MAPK inhibitor SB on IS in pig myocardium are shown in Figs. 2 and 3. The local intramyocardial infusion of SB203580 (40 nM) for 60 min before index ischemia (group II) significantly reduced infarct size from 69.3 ± 2.7% (control, group I) to 36.8 ± 3.7% (p < 0.002; Fig. 3). When SB was infused intravenously (5 mg/animal) for 10 min before the onset of 60-min coronary occlusion (group III), we also observed a significant reduction of IS as compared with control (group I; 36.1 ± 5.6% for SB, 69.3 ± 2.7% for control). The remaining infarcts were not solid but rather spotty. Important also is the fact that both local and systemic infusions of KHB/DMSO (0.1% DMSO in KHB, negative control) before index ischemia did not influence the IS as compared with control (Fig. 3). The effect of SB203580 on ischemic preconditioning [4] The effect of local and systemic infusion of SB on cardioprotection by ischemic preconditioning is shown in Figs. 4 and 5. When SB was applied locally before and during the ischemic preconditioning protocol (group VI), the IS represented 3.8 ± 0.5%. This IS was significantly lower than that in control 2 (group IV; IS, 54.0 ± 2.5%) and was not different from group V (IS, 2.5 ± 0.7%; Fig. 5). Systemic application of SB203580 before and during the preconditioning protocol (group VII) did not influence the IS limitation mediated by ischemic preconditioning (3.2 ± 0.5% for SB systemic; Fig. 5). Also in this case, IS was significantly lower than in the control group 2 (group IV). These results show that the infusion (local or systemic) of SB before and during ischemic preconditioning did not influence the IS limitation mediated by ischemic preconditioning. The infusion of KHB/DMSO before and during the preconditioning protocol did not influence the effect of ischemic preconditioning (Fig. 5). Effect of SB203580 on p38-MAPK activities [4] The p38-MAPK activity and the phosphorylation state of this enzyme were investigated during index ischemia that followed the systemic infusion of SB or of the solvent. The ventricular drill biopsies were taken from the ischemic and nonischemic regions at time points described in the experimental protocol VIII (Fig. 1). Using an antibody that reacts specifically with dual-phosphorylated p38-MAPK (Thr180/Tyr182), we investigated the content of phosphorylated p38-MAPK after systemic infusion. In both SB and KHB infusion, we found a significant increase of phospho-p38-MAPK during ischemia (Fig. 6A and B), with a maximum reached at 20 min of ischemia and without significant differences between KHB- and SB-treated tissue. Only at 30 and 45 min of ischemia did SB significantly reduce the content of phospho-p38-MAPK. With an antibody that reacts specifically with the phosphorylated form of SAPK/JNKs, we did not detect significant changes in phosphorylation of these kinases during ischemia after SB or KHB treatment (Fig. 6C). Western blot assay with a specific p38-MAPK antibody showed that there were no significant changes in p38-MAPK abundance when cytosolic fractions from untreated, KHB-, and SB-treated tissue were compared (Fig. 7A and B). Some decrease in content of p38-MAPK after SB infusion was observed after 45 min of ischemia, but this difference was not statistically significant. By means of in-gel phosphorylation of a specific p38-MAPK substrate (GST-MAPKAPK-246-400), we investigated the effect of SB on p38-MAPK activity. We found that systemic infusion of SB for 10 min before index ischemia did not significantly change the p38-MAPK activities when compared with KHB (DMSO) infusion ≤20 min of ischemia (Fig. 8A and B). Only at 30 and 45 min of ischemia did SB significantly reduce the activity of p38-MAPK. The influence of SB on p38-MAPK activities during ischemia correlates with the observed time course of p38-MAPK phosphorylation (Fig. 6B). SB is an inhibitor that directly and reversibly influences the p38-MAPK. However, SB does not change the phosphorylation state of p38-MAPK itself (a factor important for activation of this enzyme), and after washout of the inhibitor by homogenization and buffer washes, the p38-MAPK is reactivated. For this reason, we investigated the p38-MAPK activities also when SB was present during the whole experimental procedure (especially by in-gel phosphorylation). In this case, we observed significant reduction of p38-MAPK activities (reduced phosphorylation of MAPKAPK-2) in the presence of SB (Fig. 8A and C). Effect of SB203580 on the phosphorylation of ATF-2 [4] To determine the in vivo effect of SB on p38-MAPK activities, we determined also the in vivo phosphorylation of activating transcription factor-2 (ATF-2). This transcription factor serves as an endogenous substrate for p38-MAPK, and we investigated its phosphorylation after systemic infusion of SB (or KHB as negative control) and during the following ischemia (group VIII; Fig. 1). We found that the presence of SB significantly inhibited the ischemia-induced phosphorylation of ATF-2 (Fig. 9). The content of phospho-ATF-2 was decreased after infusion of SB (compared with KHB control). In negative controls (KHB infusion), we observed during ischemia increased phosphorylation of ATF-2 (maximum at 20 min of ischemia), but the presence of SB prevented the ischemia-induced p38-MAPK-mediated phosphorylation of ATF-2. Western blot assays with a specific ATF-2 antibody showed that there were no significant changes in ATF-2 abundance when nuclear fractions from untreated, KHB-, and SB-treated tissue were compared. This observation proves that the changes of phospho-ATF-2 reflect the different degree of phosphorylation of this transcription factor. Proteinuria is prevented in SB203580 treated MRL/lpr mice [5] In the first three weeks (week 14 to 16), the levels of proteinuria were significantly elevated in both SB203580 treated and untreated MRL/lpr mice compared with that in C57BL/6 mice (p < 0.05). At the end of three weeks of treatment (week 17), the level of proteinuria of group 2 and group 3 was approximative. After four weeks of treatment (week 18), the proteinuria level of group 3 declined markedly and became similar to group 1 at 21 and 22 weeks of age, indicating that SB203580 protected MRL/lpr mice from proteinuria (Fig. 1). From 14 to 22 weeks of age, decrease in urinary protein was obvious in group 3, whereas urinary protein in group 2 maintained at a high level in the whole process. In addition, over the course of 18 to 22 weeks of age, urinary protein was significantly reduced in group 3 compared with that in group 2 (p < 0.05). ALT and AST are not influenced by SB203580 in MRL/lpr mice [5] No significant difference of ALT level was found among group 1 (32.45 ± 1.20 U/L), group 2 (35.98 ± 1.82 U/L) and group 3 (34.51 ± 1.52 U/L) (p > 0.05). The level of AST was significantly elevated in group 2 (99.23 ± 7.75 U/L) and group 3 (97.54 ± 8.84 U/L) compared with group 1 (64.38 ± 5.71 U/L) (p < 0.05), whereas no significant difference was found between group 2 and group 3 (p > 0.05). BUN but not Cr is decreased in SB203580 treated MRL/lpr mice [5] SB203580 reduced BUN level in MRL/lpr mice. The BUN and Cr levels in serum of group 1 (15.86 ± 0.46 mg/dl, 51.01 ± 1.43 μmol/L) were significantly elevated compared with group 2 (10.00 ± 0.56 mg/dl, 45.95 ± 0.75 μmol/L) and group 3 (7.16 ± 0.34 mg/dl, 44.67 ± 1.27 μmol/L) (p < 0.05). The BUN level of group 3 was significantly decreased compared with group 2 (p < 0.05), but no significant difference of Cr level was found between the two groups (p > 0.05). Renal but not splenic weight is reduced in SB203580 treated MRL/lpr mice [5] SB203580 decreased kidney/body weight ratio in MRL/lpr mice. The kidney/body weight ratio in group 2 (0.0115 ± 0.0004) was significantly elevated compared with that in group 1 (0.0105 ± 0.0004) and group 3 (0.0104 ± 0.0002) (p < 0.05), whereas no significant difference was found between group 1 and group 3 (p > 0.05). The spleen/body weight ratio in group 2 (0.0125 ± 0.0020) and group 3 (0.0126 ± 0.0020) was significantly elevated than group 1 (0.0034 ± 0.0002) (p < 0.05), whereas no significant difference was found between group 2 and group 3 (p > 0.05). Renal pathologic changes are attenuated in SB203580 treated MRL/lpr mice [5] In the kidneys of group 1 (Fig. 2A), the glomerular capillary loops were thin and delicate, and endothelial and mesangial cells were normal in number and surrounded with normal tubule structures. The kidneys of group 2 (Fig. 2B) exhibited moderate to severe proliferative glomerulonephritis (endocapillary proliferation, extracapillary proliferation, focal necrosis and crescent) and interstitial damage (mononuclear cells infiltration in interstitial fields) (Fig. 2C). On the contrary, renal pathologic changes were comparatively relieved in group 3 (Fig. 2D). The numbers of intraglomerular cells (Fig. 3A) and interstitial infiltrative cells (Fig. 3B) were decreased in group 3 compared with those in group 2 (p < 0.05), whereas the number of intraglomerular red blood cells (Fig. 3C) was increased (p < 0.05). The percentage of crescents (Fig. 3D) was significantly decreased simultaneously in group 3 (p < 0.05). However, the mice in group 3 still had significant renal pathologic changes in comparison with group 1 (p < 0.05). |
| Enzyme Assay |
Cellular receptor kinase phosphorylation assay: 4μg of sheep anti-PKBα is immobilized on 25 μL of protein G-Sepharose overnight (or 1.5 hours) and washed in Buffer A (50 mm Tris, pH 7.5, 1 mm EDTA, 1 mm EGTA, 0.5 mm Na3VO4, 0.1% β-mercaptoethanol, 1% Triton X-100, 50 mm sodium fluoride, 5 mm sodium pyrophosphate, 0.1 mm phenylmethylsulfonyl fluoride, 1 μg/mL aprotinin, pepstatin, leupeptin, and 1 μm microcystin). The immobilized anti-PKB is then incubated with 0.5 ml of the lysate (from 5 × 106 cells) for 1.5 hours, washed five times in 0.5 mL of Buffer A supplemented with 0.5 m NaCl, twice in 0.5 mL of Buffer B (50 mm Tris-HCl, pH 7.5, 0.03% (w/v) Brij-35, 0.1 mm EGTA, and 0.1% β-mercaptoethanol), and twice with 100 μl of assay dilution buffer; 5× assay dilution buffer is 100 mm MOPS, pH 7.2, 125 mm β-glycerophosphate, 25 mm EGTA, 5 mm sodium orthovanadate, 5 mm DTT. The PKB enzyme immune complex is supplemented with 10 μL of assay dilution buffer, 40 μm of protein kinase A inhibitor peptide, 100 μm of PKB-specific substrate peptide, and 10 μCi of [γ-32P]ATP. The reaction is allowed to proceed for 20 minutes at room temperature while being shaken, after which the samples are pulse spun and 40 μL of the reaction volume are transferred to another tube into which 20 μL of 40% trichloroacetic acid is added to stop the reaction. After mixing and incubating at room temperature for 5 minutes, 40 μL of the mixture is transferred onto P81 phosphocellulose paper and allowed to bind for 30 seconds. The P81 piece is cleaned in acetone at room temperature after being washed three times in 0.75% phosphoric acid. The incorporation of γ-32P is then quantified using scintillation counting.
Kinase Assays [1] PKB Kinase Assay [1] Cells were lysed in Buffer A (see below) for Western blotting and PKB kinase assays. Kinase assays were performed according to the manufacturer's instructions. Briefly, 4 μg of sheep anti-PKBα was immobilized on 25 μl of protein G-Sepharose overnight (or 1.5 h) and washed in Buffer A (50 mm Tris, pH 7.5, 1 mm EDTA, 1 mmEGTA, 0.5 mm Na3VO4, 0.1% β-mercaptoethanol, 1% Triton X-100, 50 mm sodium fluoride, 5 mm sodium pyrophosphate, 0.1 mmphenylmethylsulfonyl fluoride, 1 μg/ml aprotinin, pepstatin, leupeptin, and 1 μm microcystin). The immobilized anti-PKB was then incubated with 0.5 ml of lysate (from 5 × 106 cells) for 1.5 h and washed three times in 0.5 ml of Buffer A supplemented with 0.5 m NaCl, two times in 0.5 ml of Buffer B (50 mm Tris-HCl, pH 7.5, 0.03% (w/v) Brij-35, 0.1 mm EGTA, and 0.1% β-mercaptoethanol), and twice with 100 μl of assay dilution buffer; 5× assay dilution buffer is 100 mm MOPS, pH 7.2, 125 mmβ-glycerophosphate, 25 mm EGTA, 5 mm sodium orthovanadate, 5 mm DTT. To the PKB enzyme immune complex was added 10 μl of assay dilution buffer, 40 μm protein kinase A inhibitor peptide, 100 μm PKB-specific substrate peptide, and 10 μCi of [γ-32P]ATP, all made up in assay dilution buffer. The reaction was incubated for 20 min at room temperature with shaking, then samples were pulse spun, and 40 μl of reaction volume were removed into another tube to which was added 20 μl of 40% trichloroacetic acid to stop the reaction. This was mixed and incubated for 5 min at room temperature, and 40 μl was transferred onto P81 phosphocellulose paper and allowed to bind for 30 s. The P81 pieces were washed three times in 0.75% phosphoric acid then in acetone at room temperature. γ-32P incorporation was then measured by scintillation counting. PI 3-Kinase Assay [1] Cells were lysed in PI 3-kinase lysis buffer (40 mm Tris-HCl, pH 7.5, 200 mm NaCl, 1 mm EGTA supplemented with 1 mm DTT, 1 mm Na3VO4, and 10 μg/ml each of aprotinin, pepstatin, leupeptin) at 10 × 106cells/ml, and the post-nuclear lysate was precleared with 25 μl of protein G-Sepharose for 1 h then preincubated with 5 μg of monoclonal anti-p85α (U5) and further with 25 μl of protein G-Sepharose for the final 1 h. The pellets were washed three times in 0.5 ml of PI 3-kinase assay buffer. The pellet was then resuspended in 25 μl of kinase assay buffer. To this, 10 μl of a 1 mg/ml mixture of phosphatidylinositol and phosphatidylserine (made up in 100 mm HEPES, pH 7.5, and sonicated just before use) was added. The mixture was then preincubated at room temperature for 10 min, and the reaction was started by the addition of 15 μl of ATP mixture (340 μl of water, 4.2 μl of 1 mMgCl2, 16 μl of 100 mm ATP) supplemented with 5 μCi of [γ-32P]ATP. The reaction proceeded for 15 min and was stopped by the addition of 100 μl of 1 m HCl and vortexing, adding a further 200 μl of a 1:1 chloroform:methanol and vortexing again, and microfuge-spinning the tubes for 5 min. The lower layer was removed and dried in vacuo (or at 60 °C on dry block) then redissolved in 10 μl of 4:1 chloroform:methanol before spotting onto silica plates. The plate was developed in a preequilibrated vertical tank with chloroform, methanol, 28% ammonium hydroxide, water (180:140:10.8:27.5) for 3 h (or overnight) followed by phosphorimaging analysis. p70S6 Kinase Assay [1] Cells were lysed in 0.5 ml of p70S6 kinase lysis buffer (10 mm potassium phosphate, pH 7.05, 0.5% Triton X-100, 1 mm EDTA, 5 mm EGTA, 1 mm Na3VO4, 1 mmphenylmethylsulfonyl fluoride, 10 μg/ml leupeptin, 1 μg/ml pepstatin, 1 μg/ml aprotinin), and the postnuclear lysate was precleared with 20 μl of protein A-agarose for 30 min. The precleared supernatant was then preincubated with 5 μl of rabbit antiserum to p70S6 kinase for 1 h and additionally with 25 μl of protein A-agarose with mixing for a further 1 h, all at 4 °C. The final immune complex was washed twice in 0.5 ml of lysis buffer and twice in 0.5 ml of kinase assay buffer (50 mm MOPS, pH 7.2, 1 mm DTT, 30 mm ATP, 5 mmMgCl2, 10 mm p-nitrophenylphosphate). To washed immune complex pellet was added 45 μl of assay mixture (made up of 35 μl of kinase assay buffer, 5 μl of 125 mm substrate peptide (KKRNRTLTK), 5 μl of 50 μm protein kinase A inhibitor, 5 μCi of [γ-32P]ATP), and the reaction was allowed to continue for 30 min at room temperature. The reaction was stopped by the addition of reducing sample buffer and boiling for 5 min. After separation on a peptide gel as described before (15), radioactivity incorporated into peptide was quantitated by phosphorimaging. Recombinant PDK1/PKB Assays [1] Lipid vesicles were made by drying down a mixture of phosphatidylcholine and phosphatidylserinein vacuo and reconstituting with lipid buffer (0.2m NaCl, 20 mm HEPES, 2 mm EGTA) to a final 5 times working stock (500 μmphosphatidylcholine, 500 μm phosphatidylserine, and 100 μm phosphatidylinositol 3,4,5-trisphosphate (PIP3) and sonicated before use. EE-tagged recombinant PDK1 and PKBα (both >98% pure) were prediluted in enzyme dilution buffer (1 mm DTT, 0.1 m NaCl, 1 mm EGTA, 20 mm HEPES). PDK1 assays were performed with 1 μm EE-PKB and 50 nm EE-PDK1 in the presence of appropriately diluted lipid vesicles, 0.5 μm ATP, and 1 μCi of [γ-32P]ATP in assay buffer (8 mmMgCl2, 0.12 m NaCl, 1.2 mm DTT, 1.2 mm EGTA, 0.01% azide) supplemented with protease inhibitors (1 mm phenylmethylsulfonyl fluoride, 10 μg/ml aprotinin, 10 μg/ml leupeptin) in a final volume of 5 μl. The reaction was allowed to continue for 5 min at 30 °C and stopped by boiling with 10 μl of 1.5 times SDS sample buffer (with 5 mm EDTA). The PKB autokinase assays were performed as above for PDK1 but in the absence of PDK1 and PIP3. Samples were then resolved on a 10% SDS-polyacrylamide electrophoresis gel and quantitated by phosphorimaging. |
| Cell Assay |
In order to rest CT6 cells and BA/F3 F7 cells, they are washed three times in RPMI and cultured for an overnight period in RPMI with 5% fetal calf serum without the addition of growth factors, antibiotics, or β-mercaptoethanol. Preincubation with SB203580 or a vehicle control is carried out on 2 mL of RPMI, 5% fetal calf serum and 2–5 × 106 rested CT6 cells, as shown in the figure legends. Afterward, cells are stimulated for 5 minutes at 37 °C with 20 ng/ml recombinant human IL-2, pelleted in a minifuge for 30 seconds, the medium is aspirated, and the pellet is lysed in the proper buffer. BA/F3 cells are maintained in glutamine-containing RPMI that is additionally supplemented with 5% fetal calf serum and 0.2 μg/mL G418 and stably express deletion mutants of the IL-2 receptor β chain. The cells are then thoroughly washed, allowed to rest for the night, and then washed once more before being activated with IL-2. Such cell preparations contain >90% T cells. The incorporation of [3H]thymidine is measured in cellular proliferation assays.
Cells and Proliferation Assay [1] The IL-2-dependent murine T cell line, CT6, was grown and maintained as described previously. These cells were rested by washing three times in RPMI and culturing overnight in RPMI, 5% fetal calf serum in the absence of growth factor, antibiotics, or β-mercaptoethanol supplements. 2–5 × 106 rested CT6 cells were resuspended in 2 ml of RPMI, 5% fetal calf serum and preincubated with inhibitors or vehicle control as indicated in figure legends. Cells were then stimulated with 20 ng/ml recombinant human IL-2 for 5 min at 37 °C and pelleted in a minifuge for 30 s, medium was aspirated, and the pellet was lysed in the appropriate buffer. BA/F3 cells stably expressing deletion mutants of IL-2 receptor β chain were maintained in glutamine containing RPMI further supplemented with 5% fetal calf serum and 0.2 μg/ml G418 as described previously. Human peripheral blood mononuclear cells were prepared from buffy coat leukophoresis residues and activated with 50 ng/ml OKT3 for 48 h. The cells were then washed extensively, rested overnight, and washed again before activating with IL-2; such cell preparations were >90% T cells. Cellular proliferation assays were performed by measurement of [3H]thymidine incorporation as described previously. Transient transfection assays [2] The luciferase reporter plasmid pIL6luc(-122) and the CAT reporter plasmid p(TRE)5CAT were transfected into TF-1 cell line by means of electroporation. Prior to transfection, cells were cultured for 16 h at a density of 0.5×106 cells ml−1 in the appropriate medium, washed twice and resuspended in RPMI 1640 at a density of 10×106 in 200 μl. When transfected with a single plasmid, 25 μg of DNA was added and the mixture was left at room temperature for 15 min. Cotransfections were performed with 15 μg of the reporter plasmid pIL6luc(-122) together with 15 μg of the dominant-negative expression plasmids (pRSV-MKK3(Ala), pcDNA3-MKK6(K82A), pRSV-NΔRaf1, pcDNA3-MKK4(Ala), pcDNA3-Flag-JNK1, or pcDNA3 (empty vector). Cotransfections of pGAL4tkluc (5 μg) with either pGAL4p65 (5 μg) or pGAL4dbd (5 μg) were performed under similar conditions. In addition, cells were cotransfected with 2 μg of a CMV-CAT plasmid, to normalize for transfection efficiency. Electroporation, in 0.4 cm electroporation cuvettes, was performed at 240 V and 960 μF with Gene Pulser electroporator. After electroporation, the cells were replated in RPMI 1640 containing 2% FBS. Six hours after transfection cells were stimulated for 24 h with medium or OA (30 ng ml−1) or SB203580 for 30 min prior to OA stimulation. The cells were then harvested and lysed by commercially available luciferase lysis buffer. One-hundred μl of lysis product was added to 100 μl of luciferase assay reagents and luciferase activity was measured with the Anthos Lucy1 luminometer. CAT reporter activity of 100 μl lysis product plus 100 μl CAT dilution buffer was determined with a commercially available CAT Elisa kit. Western blotting for p38, JNK1/2, and ERK1/2 [2] Phosphorylation of p38, JNK1/2, and ERK1/2 was analysed by Western blotting. Briefly, TF-1 cells were cultured for 16 h in RPMI 1640 containing 0.1% FBS and subsequently stimulated for various periods of time with medium or OA (30 ng ml−1) or SB203580 plus OA. After harvesting, total cell extracts were prepared by resuspending the cells in 500 μl 1× sample buffer (containing 2% SDS, 10% glycerol, 2% β-mercaptoethanol, 60 mM Tris-HCl (pH 6.8) and bromophenol blue) and lysing the cells by passing them through a 23G1 needle (three times). Cell extracts were directly boiled for 10 min and stored at −20°C. Before loading, samples were again boiled for 5 min and cell extracts were resolved by running 1/10th volume on a SDS/12.5%PAGE gel (acryla-mide:bisacrylamide is 173:1) and transferred to cellulosenitrate membrane. Detection of autophagy by pEGFP-LC3 [3] HCC cells were transfected with pEGFP-LC3 to measure autophagy level. Lipofectamine 2000 was employed to transfect HCC cells. Following the induction of autophagy by SB203580, the cellular localization pattern of GFP-LC3 was photographed using the Zeiss fluorescence microscope. GFP-LC3 is a highly specific fluorescence marker of autophagy and can be used to measure autophagy. When autophagy occurs, the percentage of GFP-LC3-positive cells with GFP-LC3 punctate dots increases and the dots redistribute from a diffuse pattern to a punctate cytoplasmic pattern (GFP-LC3 dots) that specifically labels preautophagosomal and autophagosomal membranes. Down-regulation of DAPK and p53 by siRNA [3] Cells were transfected with different siRNAs and control siRNA using lipofectamine 2000. Before transfection, cells were seeded in 6-well plates or 60 mm culture dishes containing DMEM medium without antibiotics for 24 h. Cells were transfected with 100 pmol siRNA in each well. The transfected cells were treated with SB203580 for 24 h. The target proteins were measured by Western blot 24 h post-transfection. |
| Animal Protocol |
Systemic lupus erythematosus (SLE) are established in female MRL/lpr mice and female C57BL/6 mice
0.1 M/day Orally administered Animal preparation Male castrated German landrace-type domestic pigs (32.6 ± 2.3 kg) were premedicated with azaperone (2 mg/kg of body weight, i.m.) and 2 mg/kg BW piritramide, s.c., 30 min before the initiation of anesthesia with 10 mg/kg BW metomidate. After tracheal intubation, a bolus of α-chloralose (25 mg/kg) was given intravenously. Anesthesia was maintained by a continuous intravenous infusion of α-chloralose (25 mg/kg/h). The animals were ventilated artificially with a pressure-controlled respirator with room air enriched with 2 L/min of oxygen. Arterial blood gases were analyzed frequently to guide adjustment of the respirator settings. Additional doses of piritramide (10 mg) were given i.v. every 60 min. Both internal jugular veins were cannulated with polyethylene tubes for administration of saline, piritramide, and α-chloralose. Arterial sheath catheters (7F) were inserted into both carotid arteries. To measure arterial blood pressure, the left sheath was advanced into the aortic arch and connected with a Statham transducer. After a midsternal thoracotomy, the heart was suspended in a pericardial cradle. Arterial pressure, heart rate, and the ECG were continuously monitored and recorded on the hard disk of a MacLab computer. A loose reversible ligature was placed halfway around the left anterior descending artery (LAD), and was subsequently tightened to occlude the vessels. In pigs subjected to intramyocardial microinfusion, eight 26-gauge needles connected by tubing with a peristaltic pump were placed in pairs along the LAD into the myocardium perpendicular to the epicardial surface. After preparation, a stabilization period of 30 min was allowed and the experimental protocols were started. The p38-MAPK inhibitor, SB203580 (abbreviated as SB), was dissolved in DMSO and finally diluted in Krebs-Henseleit buffer (KHB; final concentration of DMSO was 0.1%). For this reason, the infusion of KHB with DMSO served as a negative control (KHB). Experimental groups This study consisted of eight experimental groups (Fig. 1). Group I was subjected to 60 min of occlusion and 60 min of reperfusion (control group 1). In group II, SB203580 (40 nM) or KHB (with 0.1% DMSO) was administered by local infusion for 60 min before the index ischemia of 60 min and the following reperfusion period of 60 min. In group III, SB203580 (5 mg/animal) or KHB was applied by systemic infusion for 10 min before the index ischemia (60 min occlusion and 60 min reperfusion periods). In group IV, the animals were subjected to 40 min of occlusion followed by 60 min of reperfusion (control group 2). In group V, the animals were subjected to the preconditioning protocol (two cycles of 10-min ischemia and 10-min reperfusion) followed by a period of 40-min index ischemia and 60 min of reperfusion. In group VI, SB203580 (40 nM) or KHB was administered by local microinfusion for 15 min before the brief occlusions/reperfusions and during reperfusion periods of the preconditioning protocol. This was followed by 40 min of ischemia and 60 min of reperfusion. In group VII, SB203580(5 mg/animal) or KHB was applied by intravenous infusion for 15 min before the brief occlusions/reperfusions and during reperfusion periods of the preconditioning protocol. This was followed by 40 min of index ischemia and 60 min of reperfusion. In group VIII, SB203580 (5 mg/animal) or KHB was applied by intravenous infusion for 10 min before the index ischemia of 60 min, and left ventricular biopsies for in vitro assays were obtained at the end of SB203580 and KHB infusion and at 5, 10, 20, 30, 45, and 60 min of the following index ischemia. Drill biopsies were taken from control tissue, KHB-, and SB203580-treated tissue (Fig. 1). Biopsies weighed ∼80 mg and were ∼4 mm long (i.e., they reached from epi- to midmyocardium). Female MRL/lpr mice were randomized into two groups (n = 10 per group) and were fed control diet (named as group 2 in the following) or diet with SB203580 (named as group 3 in the following) starting at the age of 14 weeks and continuing for up to 22 weeks. Adezmapimod (SB203580) was dissolved in drinking water (250 μmol/L), was orally administered (0.4 ml/day). Ten C57BL/6 female mice were used as negative controls (named as group 1 in the following). Two mice in MRL/lpr group 2 were dead at 16 weeks and 18 weeks of age respectively. Two mice in MRL/lpr group 3 were dead at 19 weeks of age. Significant increase of urine protein (300–2000 mg/dl) was found in each mouse before death, indicating a probable renal failure be the cause of death. Ultimately, 10 mice in group 1, 8 mice in group 2 and group 3 were included in statistical analysis.[5] Systemic lupus erythematosus (SLE) is an autoimmune disease accompanying excessive inflammatory responses in a wide range of organs. Abnormal activation of p38 MAPK has been postulated to contribute to the inflammation of SLE, leading to progressive tissue and organ damages to develop lupus nephritis and autoimmune hepatitis. In order to determine whether p38 MAPK inhibitor is effective in mouse model of SLE, a specific inhibitor of p38 MAPK Adezmapimod (SB203580) was orally administrated to MRL/lpr mice aged from 14 to 22 weeks. Renal and hepatic functions, as well as pathologic changes of important organs including kidney, liver and spleen of MRL/lpr mice were evaluated. As a result, we showed that SB203580 improved renal function by decreasing the levels of proteinuria and serum BUN, ameliorating the pathologic changes of kidney and reducing Ig and C(3) depositions in the kidney. Hepatocytes necrosis, recruitment and proliferation of leucocytes in liver and spleen were found to be inhibited by administration of SB203580. Therefore, p38 MAPK activation may be partially responsible for escalating autoimmune renal, hepatic and splenic destruction, and its inhibitor may lighten the autoimmune attack in these important organs and improve renal function. Our study reveals that the selective blockade of p38 MAPK is effective to prevent and treat the disease in this model of SLE.[5] |
| ADME/Pharmacokinetics |
1. Solubility & Formulation
o Solubility: SB203580 is highly soluble in DMSO (43 mg/mL or 113.92 mM) but insoluble in water and ethanol. o Formulation: Typically supplied as a powder or in DMSO solution for research use. 2. Absorption & Bioavailability o Oral Administration: In animal studies, SB203580 was administered orally (e.g., dissolved in drinking water at 250 μM) and showed efficacy in disease models. o Intraperitoneal (IP) Injection: Used in mice at 5 mg/kg/day, demonstrating systemic activity. 3. Metabolism & Half-Life o Metabolic Stability: No direct data on metabolic pathways, but storage conditions (-20°C, protected from light) suggest sensitivity to degradation. o In Vivo Efficacy: Effective in inhibiting inflammatory cytokines in mice and rats at doses of 15–60 mg/kg, with IC50 values of 15–25 mg/kg in vivo. 4. Distribution & Protein Binding o Cell Permeability: SB203580 is cell-permeable, allowing intracellular inhibition of p38 MAPK (IC50 = 600 nM in cells). o Tissue Effects: Reduces inflammation in collagen-induced arthritis and endotoxin shock models, indicating broad tissue distribution. 5. Excretion & Clearance o No specific data on excretion pathways, but its effects in animal models suggest moderate clearance (e.g., daily dosing required for sustained activity) |
| Toxicity/Toxicokinetics |
1. Acute Toxicity & Safety Hazards
• Oral Toxicity: Classified as Acute Toxicity Category 4 (Hazard Statement H302)—harmful if swallowed • Ocular Toxicity: Causes severe eye damage (Category 1, H318); direct contact requires immediate rinsing and medical attention • Handling Precautions: Requires protective gear (gloves, goggles, masks) due to risks of inhalation or skin contact ________________________________________ 2. In Vivo Toxicity Studies Ocular Exposure (Conjunctival Injection) • Study: Subconjunctival injection of 50 μM SB203580 in rats showed no significant corneal toxicity (e.g., intact epithelium, normal stromal arrangement) but caused transient conjunctival anemia that resolved within 24 hours • Conclusion: Low toxicity for short-term ocular applications, though local irritation may occur Systemic Administration • Asthma Model: In smoke-exposed asthmatic rats, SB203580 reduced airway inflammation and improved lung function without reported adverse effects at tested doses • Pancreatitis Model: Inhibited TNF-α and pancreatic acinar cell apoptosis in severe acute pancreatitis rats, suggesting therapeutic potential with no overt toxicity noted ________________________________________ 3. Biochemical & Cellular Toxicity • Off-Target Effects: At high concentrations (>10 μM), SB203580 may non-specifically inhibit kinases like PKB or PDK1 and paradoxically activate ERK/NF-κB pathways • Cell Culture: Cytotoxicity observed in some cell lines (e.g., hepatocytes) at concentrations exceeding its p38 MAPK IC50 (0.3–0.5 μM) ________________________________________ 4. Environmental & Handling Risks • Storage: Stable at -20°C but degrades under heat, moisture, or light exposure • Disposal: Must be incinerated or handled as hazardous waste to avoid environmental contamination |
| References | |
| Additional Infomation |
SB 203580 is a member of the class of imidazoles carrying 4-methylsulfinylphenyl, 4-pyridyl and 4-fluorophenyl substituents at positions 2, 4 and 5 respectively. An inhibitor of mitogen-activated protein kinase. It has a role as an EC 2.7.11.24 (mitogen-activated protein kinase) inhibitor, a Hsp90 inhibitor, a neuroprotective agent, an EC 2.7.11.1 (non-specific serine/threonine protein kinase) inhibitor and a geroprotector. It is a member of imidazoles, a member of monofluorobenzenes, a member of pyridines and a sulfoxide.
4-(4-Fluorophenyl)-2-(4-methylsulfinylphenyl)-5-(4-pyridyl)-1H-imidazole has been reported in Annulohypoxylon truncatum, Eleutherococcus divaricatus, and other organisms with data available. Pyridinyl imidazole inhibitors, particularly SB203580, have been widely used to elucidate the roles of p38 mitogen-activated protein (MAP) kinase (p38/HOG/SAPKII) in a wide array of biological systems. Studies by this group and others have shown that SB203580 can have antiproliferative activity on cytokine-activated lymphocytes. However, we recently reported that the antiproliferative effects of SB203580 were unrelated to p38 MAP kinase activity. This present study now shows that SB203580 can inhibit the key cell cycle event of retinoblastoma protein phosphorylation in interleukin-2-stimulated T cells. Studies on the proximal regulator of this event, the phosphatidylinositol 3-kinase/protein kinase B (PKB)(Akt/Rac) kinase pathway, showed that SB203580 blocked the phosphorylation and activation of PKB by inhibiting the PKB kinase, phosphoinositide-dependent protein kinase 1. The concentrations of SB203580 required to block PKB phosphorylation (IC(50) 3-5 microM) are only approximately 10-fold higher than those required to inhibit p38 MAP kinase (IC(50) 0.3-0.5 microM). These data define a new activity for this drug and would suggest that extreme caution should be taken when interpreting data where SB203580 has been used at concentrations above 1-2 microM.[1] In the present study we investigated a possible role for the p38 mitogen-activated protein (MAP) kinase pathway in mediating nuclear factor-kappa B (NF-kappaB) transcriptional activity in the erythroleukaemic cell line TF-1. TF-1 cells stimulated with the phosphatase inhibitor okadaic acid (OA) demonstrated enhanced NF-kappaB and GAL4p65-regulated transcriptional activity which was associated with elevated p38 phosphorylation. However, pretreatment with the p38 MAPK specific inhibitor SB203580 (1 microM) or overexpression of kinase-deficient mutants of MKK3 or MKK6 did not affect OA-enhanced NF-kappaB transcriptional potency, as determined in transient transfection assays. In fact, 5 and 10 microM SB203580 enhanced rather than inhibited NF-kappaB-mediated promoter activity by 2 fold, which was independent of phosphorylation of the p65 subunit. The SB203580-mediated increase in NF-kappaB transcriptional activity was associated with enhanced phosphorylation of extracellular signal-regulated kinase (ERK)1/2 and c-Jun N-terminal kinase (JNK), but not p38 kinase. Overexpression of kinase-deficient mutants belonging to the ERK1/2, JNK, and p38 pathways showed that only dominant-negative Raf-1 abrogated SB203580-enhanced NF-kappaB activity. This would implicate the involvement of the ERK1/2 pathway in the enhancing effects of SB203580 on NF-kappaB-mediated gene transcription. This study demonstrates that the p38 MAP kinase pathway is not involved in the OA-induced activation of NF-kappaB. SB203580 at higher concentrations activates the ERK pathway, which subsequently enhances NF-kappaB transcriptional activity.[2] SB203580 is a well-known inhibitor of p38 mitogen-activated protein kinase (MAPK). However, it can suppress cell proliferation in a p38 MAPK independent manner. The inhibitory mechanism remains unknown. Here, we showed that SB203580 induced autophagy in human hepatocellular carcinoma (HCC) cells. SB203580 increased GFP-LC3-positive cells with GFP-LC3 dots, induced accumulation of autophagosomes, and elevated the levels of microtubule-associated protein light chain 3 and Beclin 1. It stimulated the phosphorylation of adenosine monophosphate-activated protein kinase (AMPK) and p53, but inhibited the phosphorylation of death-associated protein kinase (DAPK). Inhibition of AMPK, p53, or DAPK attenuated SB203580-induced autophagy. AMPK activation appeared to predate the DAPK signal. The activation of both AMPK and DAPK prompted the phosphorylation of p53 and enhanced Beclin 1 expression. Neither the downregulation of p38 MAPK by its siRNA or chemical inhibitor nor the upregulation of p38 MAPK by p38 MAPK DNA transfection affected B203580-induced autophagy. Collectively, the findings demonstrate a novel function of SB203580 to induce autophagy via activating AMPK and DAPK but independent of p38 MAPK. The induction of autophagy can thus account for the antiproliferative effect of SB203580 in HCC cells.[3] We report that SB203580 (SB), a specific inhibitor of p38-MAPK, protects pig myocardium against ischemic injury in an in vivo model. SB was applied by local infusion into the subsequently ischemic myocardium for 60 min before a 60-min period of coronary occlusion followed by 60-min reperfusion (index ischemia). Infarct size was reduced from a control value of 69.3 +/- 2.7% to 36.8 +/- 3.7%. When SB was infused systemically for 10 min before index ischemia, infarct size was reduced to 36.1 +/- 5.6%. We measured the content of phosphorylated p38-MAPK after systemic infusion of SB and Krebs-Henseleit buffer (KHB; negative control) and during the subsequent ischemic period using an antibody that reacts specifically with dual-phosphorylated p38-MAPK (Thr180/ Tyr182). Ischemia with and without SB significantly increased phospho-p38-MAPK, with a maximum reached at 20 min but was less at 30 and 45 min under the influence of the inhibitor. The systemic infusion of SB for 10 min before index ischemia did not significantly change the p38-MAPK activities (compared with vehicle, studied by in-gel phosphorylation) < or =20 min of ischemia, but activities were reduced at 30 and 45 min. Measurements of p38-MAPK activities in situations in which SB was present during in-gel phosphorylation showed significant inhibition of p38-MAPK activities. The systemic infusion of SB significantly inhibited the ischemia-induced phosphorylation of nuclear activating transcription factor 2 (ATF-2). Using a specific ATF-2 antibody, we did not observe significant changes in ATF-2 abundance when nuclear fractions from untreated, KHB-, and SB-treated tissues were compared. We investigated also the effect of local and systemic infusion of SB on the cardioprotection induced by ischemic preconditioning (IP). The infusions (local or systemic) of SB before and during the IP protocol did not influence the infarct size reduction mediated by IP. The observed protection of the myocardium against ischemic damage by SB points to the negative role of the p38-MAPK pathway during ischemia.[4] In summary, we have putatively identified PDK1/PDK2 as targets for the pyridinyl imidazole p38 MAP kinase inhibitor SB203580, which could, at least in part, explain the antiproliferative effect of the drug. The observation that SB203580 can inhibit PI 3-kinase/PDK1/PKB pathway could have major implications for the interpretation of data obtained with this drug. [1] Although activation of ERK and JNK by SB203580 has not been reported before, observations in several studies may suggest the occurrence of this phenomenon. For instance, Schwenger et al. (1998) suggested that TNF-induced p38 kinase activation may exert a negative regulatory influence on the process of NFκB activation by this cytokine in COS-1 cells. At the concentration of 10 μM, SB203580 significantly prevented the ability of the drug sodium salicylate to suppress TNF-induced IκBα degradation. However, in this study it was not ruled out that SB203580 exerted its effect by activating alternate MAPK pathways and thus enhancing the degradation of IκBα. In myeloid leukaemic cells, NF-kB expression may exert its clinically unfavourable effect by enhancing the expression of cytokine genes or by inducing the expression of anti-apoptotic genes. Insight into the regulation of NF-κB in these cells may thus lead to new clinical approaches. In the present study we showed that the p38 MAP kinase pathway does not mediate the OA-induced NF-κB activation in the TF-1 haematopoietic cell line. Moreover, SB203580 stimulation may result in adverse effects, since it enhances NF-κB and ERK.[2] Nevertheless, our results appear to indicate that SB203580 induces HCC cell autophagy independent of p38 MAPK and caspase-3 via multiple channels, and none of these channels can be 100% responsible for the induction of autophagy. For example, the suppression of AMPK by compound C does not completely inhibit SB203580-induced autophagy, neither does the inhibition of DAPK nor p53. SB203580 is a well-known p38 MAPK inhibitor to block apoptosis induced by various agents. The induction of autophagy by SB203580 may provide us with some novel concepts when dealing with cancer cell death. For example, in some situations, though the apoptosis has been inhibited by SB203580, cell survival may continue to decrease. The autophagy induced by SB203580 should give a reasonable answer to this scientific puzzle, thereby helping the development of more effective treatments for cancers. [3] In this study and also in our previous experiments, we observed two bands (protein kinases) in the range of 38-45 kDa that use MAPKAPK-2 as a substrate in vitro. We investigated the specificity of the reaction for p38-MAPK by immunoprecipitation with a p38-MAPK polyclonal antibody (C-20). The antibody is specific for p38-MAPK and is not cross-reactive with p38-MAPK-beta. The same antibody was used for detection of p38-MAPK content presented in this study (see Fig. 7A). We found that the antibody reacted very strongly with a 38-kDa protein of molecular mass of (p38-MAPK) and when the immunoprecipitate was tested by in-gel phosphorylation of MAPKAPK-2, we found activity only in the range of 38 kDa. We cannot exclude the possibility that the upper band of 45 kDa represents some isoform of p38-MAPK, but our results show that SB inhibits preferentially the activity of the lower (38-kDa) band. It is known that the p38-MAPK exists in at least six isoforms (two alternative spliced isoforms α and β and isoforms τ and δ). These p38-MAPKs differ in their sensitivity to stimulation, inhibitor sensitivity, and also substrate specificity. We cannot exclude the possibility that more than one isoform of p38-MAPK is activated during myocardial ischemia. However, PC12 cells showed a selective activation of p38-MAPK-α and p38-MAPK-γ by hypoxia. Hypoxia had no effect on the activity of the β and δ isoforms. Our results obtained with SB in vitro (phosphorylation step of in-gel assay; Fig. 8A and C) show that SB fully inhibited the ischemia-induced p38-MAPK activity. It has been described that the γ and δ isoforms are resistant to inhibition by SB/SB203580. This would suggest that these two p38-MAPK isoforms (γ and δ) are not involved in the effects of SB during ischemia and in mechanisms leading to ischemic death. In conclusion, we provide detailed information about the detrimental effect of p38-MAPK activation during ischemia, which can be inhibited by SB. We have provided further evidence for our hypothesis that ischemia/reperfusion activates different signaling cascades with opposing effects on survival, of which the ERKs and the SAPK/JNKs favor survival, and the p38-MAPKs accelerate cell death. The development of future treatment strategies for ischemic syndromes may find these observations useful. [4] Collectively, p38 MAPK inhibitor may dampen the autoimmune attack in important organs and improve renal function. Furthermore, serum levels of ALT and AST were not increased in SB203580 treated MRL/lpr mice and the survival of SB203580 treated MRL/lpr mice was similar to untreated MRL/lpr mice during the experimental period, indicating no obvious adverse effects on lifespan and liver function of SB203580. In spite of the efficacy of SB203580 observed, the inhibition of p38 MAPK is not sufficient to completely prevent organ injuries due to the findings that almost all the pathological profiles analyzed in our study were not able to be recovered by SB203580 in MRL/lpr mice compared with negative control C57BL/6 mice. Further studies with a larger number of animals and other strains of lupus-prone animal models will be needed to confirm the efficacy and mechanism of the action of SB203580, as to provide its potential clinical application for human disease. Though many different p38 MAPK inhibitors have been undergoing clinical trials, none of them has yet passed accreditation successfully for the treatment of autoimmune diseases on account of safety concerns associated with potential cross reactivities with other kinases. And unfortunately adverse effects on the central nervous system and liver have been observed in phase II clinical trials of VX745 and BIRB796. But up till now, there is no report concerning the side effect of SB203580. Therefore, further investigation of SB203580 is required to verify its safety in many other systems. Evaluation of the life span and clinical improvement after treatment being discontinued is also needed. [5] |
| Molecular Formula |
C21H16FN3OS
|
|---|---|
| Molecular Weight |
377.43
|
| Exact Mass |
377.099
|
| Elemental Analysis |
C, 66.83; H, 4.27; F, 5.03; N, 11.13; O, 4.24; S, 8.49
|
| CAS # |
152121-47-6
|
| Related CAS # |
Adezmapimod hydrochloride;869185-85-3
|
| PubChem CID |
176155
|
| Appearance |
White to light yellow solid powder
|
| Density |
1.4±0.1 g/cm3
|
| Boiling Point |
615.6±55.0 °C at 760 mmHg
|
| Melting Point |
249 - 250ºC
|
| Flash Point |
326.1±31.5 °C
|
| Vapour Pressure |
0.0±1.7 mmHg at 25°C
|
| Index of Refraction |
1.715
|
| LogP |
4.1
|
| Hydrogen Bond Donor Count |
1
|
| Hydrogen Bond Acceptor Count |
5
|
| Rotatable Bond Count |
4
|
| Heavy Atom Count |
27
|
| Complexity |
500
|
| Defined Atom Stereocenter Count |
0
|
| SMILES |
S(C([H])([H])[H])(C1C([H])=C([H])C(=C([H])C=1[H])C1=NC(C2C([H])=C([H])C(=C([H])C=2[H])F)=C(C2C([H])=C([H])N=C([H])C=2[H])N1[H])=O
|
| InChi Key |
CDMGBJANTYXAIV-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C21H16FN3OS/c1-27(26)18-8-4-16(5-9-18)21-24-19(14-2-6-17(22)7-3-14)20(25-21)15-10-12-23-13-11-15/h2-13H,1H3,(H,24,25)
|
| Chemical Name |
4-[4-(4-fluorophenyl)-2-(4-methylsulfinylphenyl)-1H-imidazol-5-yl]pyridine;hydrochloride
|
| Synonyms |
RWJ 64809; PB 203580; Adezmapimod; 4-(4-Fluorophenyl)-2-(4-methylsulfinylphenyl)-5-(4-pyridyl)-1H-imidazole; 4-[4-(4-fluorophenyl)-2-(4-methylsulfinylphenyl)-1H-imidazol-5-yl]pyridine; 4-(4-(4-fluorophenyl)-2-(4-(methylsulfinyl)phenyl)-1H-imidazol-5-yl)pyridine; RWJ64809; SB203580; SB203580; SB 203580; RWJ-64809; PB-203580; PB203580
|
| HS Tariff Code |
2934.99.9001
|
| Storage |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| Solubility (In Vitro) |
|
|||
|---|---|---|---|---|
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 2.5 mg/mL (6.62 mM) (saturation unknown) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution.
Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: 2 mg/mL (5.30 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution; with ultrasonication. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 20.0 mg/mL clear DMSO stock solution to 400 μL PEG300 and mix evenly; then add 50 μL Tween-80 to the above solution and mix evenly; then add 450 μL normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. View More
Solubility in Formulation 3: 2 mg/mL (5.30 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution; with ultrasonication. Solubility in Formulation 4: 2 mg/mL (5.30 mM) in 10% DMSO + 90% Corn Oil (add these co-solvents sequentially from left to right, and one by one), clear solution; with ultrasonication. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 20.0 mg/mL clear DMSO stock solution to 900 μL corn oil and mix evenly. Solubility in Formulation 5: 4% DMSO+30% PEG 300+5% Tween 80+ddH2O: 5mg/mL Solubility in Formulation 6: 16.67 mg/mL (44.17 mM) in 0.5% CMC-Na/saline water (add these co-solvents sequentially from left to right, and one by one), suspension solution; with ultrasonication. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.6495 mL | 13.2475 mL | 26.4950 mL | |
| 5 mM | 0.5299 mL | 2.6495 mL | 5.2990 mL | |
| 10 mM | 0.2649 mL | 1.3247 mL | 2.6495 mL |
*Note: Please select an appropriate solvent for the preparation of stock solution based on your experiment needs. For most products, DMSO can be used for preparing stock solutions (e.g. 5 mM, 10 mM, or 20 mM concentration); some products with high aqueous solubility may be dissolved in water directly. Solubility information is available at the above Solubility Data section. Once the stock solution is prepared, aliquot it to routine usage volumes and store at -20°C or -80°C. Avoid repeated freeze and thaw cycles.
Calculation results
Working concentration: mg/mL;
Method for preparing DMSO stock solution: mg drug pre-dissolved in μL DMSO (stock solution concentration mg/mL). Please contact us first if the concentration exceeds the DMSO solubility of the batch of drug.
Method for preparing in vivo formulation::Take μL DMSO stock solution, next add μL PEG300, mix and clarify, next addμL Tween 80, mix and clarify, next add μL ddH2O,mix and clarify.
(1) Please be sure that the solution is clear before the addition of next solvent. Dissolution methods like vortex, ultrasound or warming and heat may be used to aid dissolving.
(2) Be sure to add the solvent(s) in order.
|
 |
 |